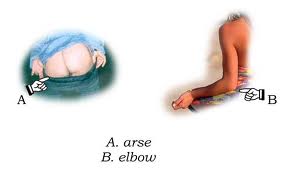
And here it is, Wednesday 3rd August, affectionately known as the Day of Death amongst seasoned nurses and senior clinicians, when all the brand new F1 doctors are let loose on the wards. Having spent five years pretending to be a doctor and one month in limbo between finals results day and officially starting work amused at being called Dr Doctor by friends and family, to find myself with vast quantities of responsibility in the form of prescription writing (as in, authorising the administration of a substance that will actually change that patient's physiology), assessing patients (as in, in order to decide what on earth to do with them) and writing in the notes (as in, without the understanding that signing off as a medical student would mean everything I had written would be entirely disregarded by anyone wanting to know something relevant about the patient). Naturally I had spent my entire month off celebrating, being on holiday, and forgetting everything I had learnt for finals. I did however find the above diagram helpful.
What I hadn't realised, was that not only were all the F1 doctors starting, all the SHOs were changing jobs as well. So everyone I had got to know during Shadowing Week (usually unpaid opportunity to practise how to look dazed and confused on ward rounds, run around in a disorganised fashion trying to find forms you have never seen nor heard of, and remind oneself what patients look (and smell) like) had disappeared and somehow I became the junior doctor that new the most about how our particular ward/hospital worked.
I found myself accosted by a nurse informing me that "the patient's heart rate has gone up". "How high?" I asked, frantically trying to remember something about this particular patient. "130". The nurse then looked at me, clearly expecting me to know what action to take. "Er.. maybe needs an ECG?" Having made the nurse look satisfied with a vaguely sensible answer she disappeared, and came back brandishing said ECG at me. Thankfully my pattern recognition kicked in and I spotted he was in fast AF. And then I found myself checking the notes for a previous ECG (it was new AF), assessing him for conscious level, SOB, chest pain and signs of shock and concluding (having checked with the friendly registrar) he was probably stable enough to go for the CT that the porters were hovering about waiting to take him down for. Cue long 40mins with intermittent imaginings of him arresting in the scanner. Wrote up digoxin and vowed to take blood (to check for electrolyte disturbances and markers of infection, did he have a CXR?). Patient returns alive and back in sinus rhythm. Crossed off digoxin and breathed sigh of relief. Maybe this whole responsibility thing wont be so bad after all..
No comments:
Post a Comment