Happened upon one of our junior staff nurses with several towels draped over her shoulders and arms, and a couple of disposable plastic aprons over her head, carrying a couple of wash bowls and some more towels along the corridor outside one of our wards.
Curious (and slightly concerned that maybe one of our patients was fountaining from some orifice), I followed her to find that the ceiling had sprung a leak outside one of the patient toilets and a positive torrent of water was coming out of it. She spread some of the towels on the floor and knelt down to place the wash bowls under the falling water.
No sooner had she positioned them there was a crack and the ceiling tile above her broke and the poor thing was deluged in slightly yellow water of questionable origin, letting out a quite understandable shriek!
I felt very sorry for her and went to find some more towels, but it was rather funny to watch! Turns out the sluice on the floor above had flooded ?cause.
On my way back along the corridor I was stopped by a lost-looking patient who asked for the way to the "maxi failure facial department". Trying to keep from chortling I directed her to Max Facs, wondering quite what she was expecting to find when she got there!
Blogsite of a brand-new FY1 doctor working in a busy DGH, designed to give those that are interested an insight into the job and a chance to learn from my experiences.
Thursday, 29 December 2011
Monday, 26 December 2011
Dr Doctor - working Christmas.
Everyone grumbles about having to work Christmas. Having never done it I wasnt sure if it would be fun, with everyone in a good mood wearing tinsel and flashing objects and other festive items of clothing, or depressing because in reality we're all trapped in a hospital away from our families. I was on twilight shifts this weekend which at least meant I could make a proper turkey lunch with my housemate before work.
A highlight of the Christmas Eve shift was when a collection of carol singers came round the elderly care wards. They really lifted the atmosphere, and it was lovely to see their number increased by a handful of pink nightdress-clad zimmer frame-wielding little old ladies whose faces lit up as they tottered out of their rooms to join in the singing. One particularly enthusiastic lady knew all the words but couldnt really carry a tune and screeched her way through 'Silent Night' drowning out most of the others. When the song finished one of the other ladies muttered "It's never a bloody silent night with her around!" The singers moved on, and I joined the nurses in fielding our little old ladies back to their rooms.
I was called to see a patient who had dropped their oxygen saturations to 83% (sit patient upright, controlled oxygen as he had COPD, ABG, CXR as chest sounded full of crackles, IV access and bloods). I diagnosed a pneumonia as his inflammatory markers were raised and his chest x-ray wasnt typical of pulmonary oedema and had evidence of bilateral consolidation, so started him on IV antibiotics. Sad thing was he had been due to go home that day, and this would be his last Christmas because he had terminal stomach cancer. It was quite hard to tell him he wouldnt be going home after all.
On Christmas Day I started off wishing my patients a Merry Christmas whenever I went to see them, which usually drew a Merry Christmas in return, but I did reflect that actually, even if it were mid August and I swept into their room with a smile and a Merry Christmas, most of them would probably think it must be Christmas.
Having taken blood from one lady who had just finished her Christmas lunch I offered to pull a cracker with her as she had one on her food tray. She was quite excited at this thought so we pulled the cracker which made a rather loud bang and a nurse come running to find a grinning little old lady and me saying "look, you've won!" The patient insisted I wear her party hat.
The shift remained relatively calm, and my SHO and I managed to sit down for a tea and mince pie break. Every ward had a LOT of food to keep us going. Finished work at 10pm and got back to hospital accommodation in time to spend the last bit of Christmas day unwinding with some mulled wine. All in all not a bad weekend
A highlight of the Christmas Eve shift was when a collection of carol singers came round the elderly care wards. They really lifted the atmosphere, and it was lovely to see their number increased by a handful of pink nightdress-clad zimmer frame-wielding little old ladies whose faces lit up as they tottered out of their rooms to join in the singing. One particularly enthusiastic lady knew all the words but couldnt really carry a tune and screeched her way through 'Silent Night' drowning out most of the others. When the song finished one of the other ladies muttered "It's never a bloody silent night with her around!" The singers moved on, and I joined the nurses in fielding our little old ladies back to their rooms.
I was called to see a patient who had dropped their oxygen saturations to 83% (sit patient upright, controlled oxygen as he had COPD, ABG, CXR as chest sounded full of crackles, IV access and bloods). I diagnosed a pneumonia as his inflammatory markers were raised and his chest x-ray wasnt typical of pulmonary oedema and had evidence of bilateral consolidation, so started him on IV antibiotics. Sad thing was he had been due to go home that day, and this would be his last Christmas because he had terminal stomach cancer. It was quite hard to tell him he wouldnt be going home after all.
On Christmas Day I started off wishing my patients a Merry Christmas whenever I went to see them, which usually drew a Merry Christmas in return, but I did reflect that actually, even if it were mid August and I swept into their room with a smile and a Merry Christmas, most of them would probably think it must be Christmas.
Having taken blood from one lady who had just finished her Christmas lunch I offered to pull a cracker with her as she had one on her food tray. She was quite excited at this thought so we pulled the cracker which made a rather loud bang and a nurse come running to find a grinning little old lady and me saying "look, you've won!" The patient insisted I wear her party hat.
The shift remained relatively calm, and my SHO and I managed to sit down for a tea and mince pie break. Every ward had a LOT of food to keep us going. Finished work at 10pm and got back to hospital accommodation in time to spend the last bit of Christmas day unwinding with some mulled wine. All in all not a bad weekend
Thursday, 22 December 2011
Dr Doctor I think I'm having a DKA!
So ward work this week has been pretty routine. For some reason they've stuck a 17 year old work experience student with me who has been, predictably, somewhat bored having to watch me fill in forms, take bloods, do cannulas, phone the lab and very occasionally interact with a patient. Tried to organise something more exciting for him like watching an operation in theatre but we were told he's too young as you have to be 18. I had forgotten how X-rated our theatres are!
So with nothing exciting to report I'll return to my last shift in MAU and reflect on a patient that actually managed to become really rather sick in the discharge bay. She was a type 1 diabetic who had come in with abdominal pain, nausea, vomiting and diarrhoea. She had been very stable and was just awaiting another speciality to review her before going home. However, she started vomiting late morning and had some more diarrhoea, her obs remained stable so I prescribed some antiemetics, checked her blood sugar (8.5) and routine bloods and decided to keep a close eye on her.
A couple of hours later the nurse called me to see her because she was having chest pain. I asked them to do an ECG which showed a sinus tachycardia at 130 with ST depression in the lateral leads. Patient at this point looked really very unwell and said she felt awful and she (and I) was worried she might be having a DKA (diabetic ketoacidosis, lack of insulin => production of ketones => these are acidic = bad). Put the patient on some oxygen and asked for a urine dip which had ketones in it, rechecked the blood sugar which was 17.5. Decided I needed a senior to be come and review before I took an ABG to check her pH (if acidotic with high blood sugar and ketones = DKA = bad).
Phoned the med reg who was spectacularly uninterested, wouldnt listen to my concerns and ordered me to take an ABG before bothering her again. reiterated that the patient looks Sick and that I was Worried about her but she hung up on me.
So I took an ABG and asked the nurses to repeat the ECG (still ST depression, probably rate related ischaemia).
pH 7.46 (slight alkalosis, definitely not an acidosis)
pCO2 3.58 (low therefore respiratory alkalosis, compensating metabolic acidosis? see base excess)
pO2 7.4 (low, need to increase oxygen)
BE -3.5 (negative base excess means there is a metabolic acidosis, likely lactate or ketones)
HCO3 21.4 (low bicarb, suggests compensating for metabolic acidosis)
O2 Sats 92.5
K+ 4.1 (anion gap = 8.6, within normal range therefore metabolic acidosis possibly not due to
Well I thought that was an interesting blood gas. The med reg didnt, and still wouldnt come to see the patient.
- I am a diabetes registrar. this is not DKA. I have patients to see in resus. Give her some morphine for the chest pain and what else do you want to do?
- I'm going to increase the rate of her IV fluids, increase her oxygen and put her on an insulin sliding scale and continue antiemetics and hopefully get you to see her then?
- Yes do that and I'll come at some point once I've seen the patients in resus.
- Er.. *click*
I was actually feeling uncharacteristically stressed at this point, more because of the reg's dismissive attitude than the patient's condition. Did the above and then was at a loss as to what to do next. Was just considering trying to find an SHO (who more than likely would have said we need the med reg, hence why I called the med reg in the first place) or a consultant when the med reg appeared. She asked the patient the exact same questions I had when I reviewed her an hour before (I know they need their own history but it was like she hadnt listened to anything I had told her) and said they would move her out of the discharge lounge to an acute bed again. Patient looked a little less sick than before so maybe I had done something right after all.
I know I'm 'only' an FY1, but I'm not an idiot and I wouldnt ask for senior help unless I'm feeling out of my depth, which I was. Generally the seniors are very supportive, and this experience was an exception to the norm, and no harm came to the patient, which is the main thing.
So with nothing exciting to report I'll return to my last shift in MAU and reflect on a patient that actually managed to become really rather sick in the discharge bay. She was a type 1 diabetic who had come in with abdominal pain, nausea, vomiting and diarrhoea. She had been very stable and was just awaiting another speciality to review her before going home. However, she started vomiting late morning and had some more diarrhoea, her obs remained stable so I prescribed some antiemetics, checked her blood sugar (8.5) and routine bloods and decided to keep a close eye on her.
A couple of hours later the nurse called me to see her because she was having chest pain. I asked them to do an ECG which showed a sinus tachycardia at 130 with ST depression in the lateral leads. Patient at this point looked really very unwell and said she felt awful and she (and I) was worried she might be having a DKA (diabetic ketoacidosis, lack of insulin => production of ketones => these are acidic = bad). Put the patient on some oxygen and asked for a urine dip which had ketones in it, rechecked the blood sugar which was 17.5. Decided I needed a senior to be come and review before I took an ABG to check her pH (if acidotic with high blood sugar and ketones = DKA = bad).
Phoned the med reg who was spectacularly uninterested, wouldnt listen to my concerns and ordered me to take an ABG before bothering her again. reiterated that the patient looks Sick and that I was Worried about her but she hung up on me.
So I took an ABG and asked the nurses to repeat the ECG (still ST depression, probably rate related ischaemia).
pH 7.46 (slight alkalosis, definitely not an acidosis)
pCO2 3.58 (low therefore respiratory alkalosis, compensating metabolic acidosis? see base excess)
pO2 7.4 (low, need to increase oxygen)
BE -3.5 (negative base excess means there is a metabolic acidosis, likely lactate or ketones)
HCO3 21.4 (low bicarb, suggests compensating for metabolic acidosis)
O2 Sats 92.5
Lactate 1.2 (normal lactate therefore metabolic acidosis not due to this ?ketones)
Glucose 15.2
K+ 4.1 (anion gap = 8.6, within normal range therefore metabolic acidosis possibly not due to
Cl- 106 ketones which would cause a raised anion gap acidosis. ?due to diarrhoea which
Na+ 136 would cause a loss of bicarb.. hmm..)Well I thought that was an interesting blood gas. The med reg didnt, and still wouldnt come to see the patient.
- I am a diabetes registrar. this is not DKA. I have patients to see in resus. Give her some morphine for the chest pain and what else do you want to do?
- I'm going to increase the rate of her IV fluids, increase her oxygen and put her on an insulin sliding scale and continue antiemetics and hopefully get you to see her then?
- Yes do that and I'll come at some point once I've seen the patients in resus.
- Er.. *click*
I was actually feeling uncharacteristically stressed at this point, more because of the reg's dismissive attitude than the patient's condition. Did the above and then was at a loss as to what to do next. Was just considering trying to find an SHO (who more than likely would have said we need the med reg, hence why I called the med reg in the first place) or a consultant when the med reg appeared. She asked the patient the exact same questions I had when I reviewed her an hour before (I know they need their own history but it was like she hadnt listened to anything I had told her) and said they would move her out of the discharge lounge to an acute bed again. Patient looked a little less sick than before so maybe I had done something right after all.
I know I'm 'only' an FY1, but I'm not an idiot and I wouldnt ask for senior help unless I'm feeling out of my depth, which I was. Generally the seniors are very supportive, and this experience was an exception to the norm, and no harm came to the patient, which is the main thing.
Monday, 19 December 2011
Dr Doctor - overworked and underpaid..
I am so very tired. My last four shifts in MAU totalled 52 hours over the weekend. That's already more than the European Working Time Directive allows, in four days! Today I was straight back to the wards, and my next day off is Boxing Day, so I'll have worked 120 hours in 11 days without a day off.
I calculated I'm actually earning less than minimum wage if I divide my salary into hourly pay, and some of the agency nurses are paid more than me to sit and read magazines, drink tea (during their protected break times, a privilege not afforded to doctors) and occasionally do a drugs round.
I find this an interesting observation, especially when the government are gearing up to *ahem* 'amend' our pension schemes, making us pay a higher percentage for a lower return, while raising the retirement age to near 70. No wonder an increasing proportion of our junior doctors are choosing to disappear overseas to practise.
I calculated I'm actually earning less than minimum wage if I divide my salary into hourly pay, and some of the agency nurses are paid more than me to sit and read magazines, drink tea (during their protected break times, a privilege not afforded to doctors) and occasionally do a drugs round.
I find this an interesting observation, especially when the government are gearing up to *ahem* 'amend' our pension schemes, making us pay a higher percentage for a lower return, while raising the retirement age to near 70. No wonder an increasing proportion of our junior doctors are choosing to disappear overseas to practise.
Friday, 16 December 2011
Dr Doctor - last MAU days
Back after 3 days off to my last set of MAU day shifts. Very long day today, I wasnt assigned to a bay so floated between all of them, doing jobs and clerking an endless stream of patients with chest pain, PR bleeding, abdominal pain and jaundice, the ubiquitous collapse?cause and 'general unwellness'.
Clerked a dear old man earlier, thought he might be delirious so applied the Abbreviated Mental Test Score (AMTS) before taking the rest of the history (a consultant once advised me that if they score really badly - as in have no idea where/who/when/what they are - then the rest of the history can be a lot shorter as everything they say is likely to be inaccurate). One of the components of the AMTS is to remember an address. Most questions I asked this chap thereafter were answered with "42 West Street" and there came a delighted screech of "42 West Street!" whenever I approached or passed the bed.
Spent a significant amount of time trying to track down a covering letter for a GP admission which had arrived with a different patient's admission letter from a different GP surgery. Finally got on the phone to the correct surgery:
- Hello, this is one of the doctors calling from MAU at the hospital, hoping to speak to one of your doctors about one of your patients we've had admitted.
- Which GP is it?
- Dr Jones.
- He's dead.
- He's dead!?
- Yes, has been for several years.
- Er..
Wasn't expecting that one!
Clerked a dear old man earlier, thought he might be delirious so applied the Abbreviated Mental Test Score (AMTS) before taking the rest of the history (a consultant once advised me that if they score really badly - as in have no idea where/who/when/what they are - then the rest of the history can be a lot shorter as everything they say is likely to be inaccurate). One of the components of the AMTS is to remember an address. Most questions I asked this chap thereafter were answered with "42 West Street" and there came a delighted screech of "42 West Street!" whenever I approached or passed the bed.
Spent a significant amount of time trying to track down a covering letter for a GP admission which had arrived with a different patient's admission letter from a different GP surgery. Finally got on the phone to the correct surgery:
- Hello, this is one of the doctors calling from MAU at the hospital, hoping to speak to one of your doctors about one of your patients we've had admitted.
- Which GP is it?
- Dr Jones.
- He's dead.
- He's dead!?
- Yes, has been for several years.
- Er..
Wasn't expecting that one!
Tuesday, 13 December 2011
Dr Doctor - MAU Twilights 2
Finished another set of twilight shifts in MAU. One of the SHOs was off sick so I got to cover a bay of patients for two shifts. The first one I ended up with the 3 sickest patients in the unit, all of whom became unwell simultaneously!
The first was a little old lady with sepsis who kept dropping her blood pressure and needed gentle fluid boluses (she also had heart failure so didnt want to send her into pulmonary oedema). She actually remained fairly stable provided she was kept sat upright (the nurses kept putting the bed head "down a little bit to make you more comfy dear" and I kept finding her gasping and tripodding herself on the edge of the bed).
The second was a lady who had come in with confusion and was about GCS 13 on admission. When I went to see her she had dropped her GCS to 7 and wasn't moving one side of her body *Erk*. She was maintaining her airway however. Phoned the med reg who was doing a lumbar puncture so went to find a consultant who said he'd "be there in a minute". Returned to my bay to find some nurses flapping because another patient (admitted with chest pain, probable costochondritis but maybe a PE) was having chest pain again, and she looked very short of breath. *Erk* (15L O2 via non rebreathe mask, urgent ECG(no acute changes), send med student running with an ABG, send nurse to find an SHO, little to find on examination, tachycardic (me, and the patient), attempt to obtain IV access).
Consultant appears and doesnt look particularly interested in this gasping patient, disappears and pokes his head round the curtains 5 mins later to declare that my GCS 7 lady is actually GCS 13 again. Med student reappears with ABG which shows a respiratory alkalosis and a PO2 of 40 (oxygenating rather well then). Patient looks much less short of breath so turn down the oxygen to 35%. Patient says chest pain has gone away and she looks back to normal. Refer for 12 hour troponin and investigation for PE.
My last shift I had one interesting patient who at first was a bit of a mystery. She had come in with shortness of breath on a background of known congestive cardiac failure, with a metallic heart valve, on warfarin. She also suffered with ischaemic heart disease and was rather overweight. It transpired she had been rather tired for several weeks, and suffered with recurrent urinary tract infections for which she had had several courses of various antibiotics. No current urinary symptoms and her stools had been darker but no PR bleeding. No recent fevers or cough. There was little to find on examination, she looked a little pale and a little breathless, possibly had a slight systolic heart murmur (and a metallic click), she also had a slightly firm left calf from where she had a recent haematoma.
So my list of differentials was quite long, anaemia, PE, ACS, endocarditis (suggested by the A&E clerking although she had no peripheral stigmata of this), hypothyroidism.. so I sent a vast array of blood tests FBC, U&E, CRP, LFT, TFT, INR, blood cultures and did an ABG which showed decreased PO2 and an Hb of 6.1. Hmm. Should have sent a group and save. Discussed with the SHO who said wait for the lab blood results to confirm anaemia. Turned out she was indeed anaemic and was transfused overnight. The cause was GI bleeding because the antibiotics for her UTIs had interfered with her warfarin metabolism giving her an INR of 7!
The first was a little old lady with sepsis who kept dropping her blood pressure and needed gentle fluid boluses (she also had heart failure so didnt want to send her into pulmonary oedema). She actually remained fairly stable provided she was kept sat upright (the nurses kept putting the bed head "down a little bit to make you more comfy dear" and I kept finding her gasping and tripodding herself on the edge of the bed).
The second was a lady who had come in with confusion and was about GCS 13 on admission. When I went to see her she had dropped her GCS to 7 and wasn't moving one side of her body *Erk*. She was maintaining her airway however. Phoned the med reg who was doing a lumbar puncture so went to find a consultant who said he'd "be there in a minute". Returned to my bay to find some nurses flapping because another patient (admitted with chest pain, probable costochondritis but maybe a PE) was having chest pain again, and she looked very short of breath. *Erk* (15L O2 via non rebreathe mask, urgent ECG(no acute changes), send med student running with an ABG, send nurse to find an SHO, little to find on examination, tachycardic (me, and the patient), attempt to obtain IV access).
Consultant appears and doesnt look particularly interested in this gasping patient, disappears and pokes his head round the curtains 5 mins later to declare that my GCS 7 lady is actually GCS 13 again. Med student reappears with ABG which shows a respiratory alkalosis and a PO2 of 40 (oxygenating rather well then). Patient looks much less short of breath so turn down the oxygen to 35%. Patient says chest pain has gone away and she looks back to normal. Refer for 12 hour troponin and investigation for PE.
My last shift I had one interesting patient who at first was a bit of a mystery. She had come in with shortness of breath on a background of known congestive cardiac failure, with a metallic heart valve, on warfarin. She also suffered with ischaemic heart disease and was rather overweight. It transpired she had been rather tired for several weeks, and suffered with recurrent urinary tract infections for which she had had several courses of various antibiotics. No current urinary symptoms and her stools had been darker but no PR bleeding. No recent fevers or cough. There was little to find on examination, she looked a little pale and a little breathless, possibly had a slight systolic heart murmur (and a metallic click), she also had a slightly firm left calf from where she had a recent haematoma.
So my list of differentials was quite long, anaemia, PE, ACS, endocarditis (suggested by the A&E clerking although she had no peripheral stigmata of this), hypothyroidism.. so I sent a vast array of blood tests FBC, U&E, CRP, LFT, TFT, INR, blood cultures and did an ABG which showed decreased PO2 and an Hb of 6.1. Hmm. Should have sent a group and save. Discussed with the SHO who said wait for the lab blood results to confirm anaemia. Turned out she was indeed anaemic and was transfused overnight. The cause was GI bleeding because the antibiotics for her UTIs had interfered with her warfarin metabolism giving her an INR of 7!
Monday, 5 December 2011
Dr Doctor "CARDIAC ARREST"
One of the other perks of MAU Nights is that you carry the crash bleep. It only went off twice this weekend.
The night before last we had been sat drinking tea in the mess (I had seized the opportunity after my haematemesis man went to theatre) and had to run to the other side of the hospital (made considerably easier by the fact it was 330am and the corridors were empty). Arrived somewhat out of breath to find one of the surgical patients being subjected to CPR and the usual accompanying flurry of activity. She was in asystole and the ITU and medical registrars made the decision to stop fairly soon after we arrived. Later found out that she had been due to go to theatre for an emergency laparotomy to relieve a probable bowel obstruction but had been sent back to the ward because our haematemesis man was prioritised ahead of her. Chances are had she made it to theatre she would have arrested on induction or on the table and would have died anyway, but had mixed feelings about it.
Last night the crash bleep went off at 630am and I had to run all the way to the same surgical ward (up several flights of stairs). This time I was running on my own and received a few strange looks from porters and cleaners on the way. Arrived to find two nurses performing CPR with rather poor technique, and noted that the one holding the airway had the facemask on the patient upside down! Rectified this and popped in an oropharyngeal airway then took over chest compressions as the med reg arrived. Patient was in pulseless electrical activity and we managed to get a pulse back on him which was a good feeling. Dont know the outcome as I returned to MAU before he was taken for a scan/to ITU.
Sat down to update the handover list near the end of the shift, somewhat tired by this point, and the healthcare assistant (HCA) next to me who was labelling some swabs said:
- How do you spell 'froat'?
- 'Froat'? Do you mean throat?
- Yeah froat.
- Er.. T-H-R-O-A-T.
- Fanks.
The night before last we had been sat drinking tea in the mess (I had seized the opportunity after my haematemesis man went to theatre) and had to run to the other side of the hospital (made considerably easier by the fact it was 330am and the corridors were empty). Arrived somewhat out of breath to find one of the surgical patients being subjected to CPR and the usual accompanying flurry of activity. She was in asystole and the ITU and medical registrars made the decision to stop fairly soon after we arrived. Later found out that she had been due to go to theatre for an emergency laparotomy to relieve a probable bowel obstruction but had been sent back to the ward because our haematemesis man was prioritised ahead of her. Chances are had she made it to theatre she would have arrested on induction or on the table and would have died anyway, but had mixed feelings about it.
Last night the crash bleep went off at 630am and I had to run all the way to the same surgical ward (up several flights of stairs). This time I was running on my own and received a few strange looks from porters and cleaners on the way. Arrived to find two nurses performing CPR with rather poor technique, and noted that the one holding the airway had the facemask on the patient upside down! Rectified this and popped in an oropharyngeal airway then took over chest compressions as the med reg arrived. Patient was in pulseless electrical activity and we managed to get a pulse back on him which was a good feeling. Dont know the outcome as I returned to MAU before he was taken for a scan/to ITU.
Sat down to update the handover list near the end of the shift, somewhat tired by this point, and the healthcare assistant (HCA) next to me who was labelling some swabs said:
- How do you spell 'froat'?
- 'Froat'? Do you mean throat?
- Yeah froat.
- Er.. T-H-R-O-A-T.
- Fanks.
Sunday, 4 December 2011
Dr Doctor he's vomiting blood again!
Last night I only had one particularly sick patient to deal with. A 77 year old gentleman who had come in with GI bleeding with a background of angiodysplasia (abnormal bood vessels in the GI tract that are likely to bleed). His haemoglobin (Hb) was 7.3 on admission and his INR was 5.7 (he was on warfarin for a metallic heart valve). He had been cross matched four units for transfusions which we started running into him.
An hour or two later around 1am he had an episode of vomiting blood. His obs were all stable at this stage but he was a little anxious (which can be one of the first signs a patient is heading into shock) so I got further IV access just in case and made my SHO aware. An hour or so after that he vomited a rather larger amount of blood and dropped his systolic blood pressure to 80 with a heart rate of 128 - scary stuff! He looked really sick at this stage, was clammy, shaky and really anxious.
Put up 500ml of gelofusine stat and called the med reg. She asked me to ring blood bank to get four units of fresh frozen plasma (FFP) and cross match another 6 units of blood before she arrived. One of the other SHOs arrived put in another cannula and took a set of bloods. I ran to A&E with a venous blood gas which showed his Hb had dropped to 6.4. We started running in the FFP and blood stat while the med reg phoned the on call endoscopist and the on call anaesthetist and ITU.
The nurses rang the patient's family and while we were waiting for the patient to go to theatre he got to talk to them. It was quite heart rending to hear him saying his goodbyes as if it might be his last.
In theatre they found several bleeding sites including one of the abnormal vessels that was actively bleeding which they injected with adrenaline (for vasoconstriction) and cauterised. He had a further 7 units of blood in theatre and the rest of the FFP. By the time he came back to MAU around 5am he was much more stable, his repeat Hb was 9.7 and his INR had come down to 2.2.
We saved this man's life.
Saturday, 3 December 2011
Dr Doctor - MAU NIghts Again
Excellent night shift last night. Started off the shift with one patient on BiPAP (non-invasive ventilation) whose blood gas results got steadily worse to the point where the med reg sent him to Respiratory Highcare.
Barely had time to breathe before noticing that one gentleman who had come in short of breath had a rapidly rising heart rate and a rapidly falling blood pressure. He was being treated for a chest infection but his inflammatory markers werent raised and he was apyrexial. He did have a very bubbly sounding chest however. Called the med reg again and we gave him a bolus of fluid. Cue much coughing up of white frothy sputum and no improvement in blood presssure. So having given him pulmonary oedema, we gave him some furosemide and he promtly dropped his BP even further. By this time he had become very confused and just looked awfully sick. Med reg phoned ITU in the end and he was whisked away to a higher place of additional monitoring.
Didnt have time to feel sad about having two very broken patients less than halfway through the shift as the man in bed 18 decided to pick that moment to go into a convincing supraventricular tachycardia with a rate of 160. He had no chest pain or shortness of breath, and no signs of shock so he wasnt compromised. Decided to try some valsalva manoeuvres with him (this raises intrathoracic pressure which activates the vagus nerve, and the parasympathetic stimulation in theory should slow the heart rate). Found myself pondering whether anybody else in the world was spending their time encouraging a 44 year old tachycardic to blow into a syringe at 4 am. Probably just me. Carotid massage didnt work either so called the med reg and we gave some adenosine. The underlying rhythm was atrial flutter, and as he hadnt spontaneously reverted to sinus rhythm the med reg sent him to the Coronary Care Unit.
To add to the fun I also had a 33 year old type 1 diabetic chap admitted with a sodium of 112 (very low) and a potassium of 5.4 (a little high). He was feeling dreadful, nauseus, dizzy on standing and we wondered if he might have Addison's disease (steroid deficiency). ECG showed peaked T waves so I treated his hyperkalaemia with IV calcium gluconate and insulin (with 50% dextrose) and he went hypo! Cue hypostop and more IV glucose.
Regarding his possible Addisons disease, his cortisol came back at 143 (lowish but not diagnostically so). We gave him some dexamethasone, a strong steroid that wouldnt affect the results of the Short Synacthen test (cortisol challenge test) in the morning. He also needed lying/standing blood pressures, an ACTH level and paired serum/urine osmolalities which I handed over to the day team.
I think I might be slightly in love with the med reg after last night. There's a good chance neither I nor the patients would have made it through last night without her!
Barely had time to breathe before noticing that one gentleman who had come in short of breath had a rapidly rising heart rate and a rapidly falling blood pressure. He was being treated for a chest infection but his inflammatory markers werent raised and he was apyrexial. He did have a very bubbly sounding chest however. Called the med reg again and we gave him a bolus of fluid. Cue much coughing up of white frothy sputum and no improvement in blood presssure. So having given him pulmonary oedema, we gave him some furosemide and he promtly dropped his BP even further. By this time he had become very confused and just looked awfully sick. Med reg phoned ITU in the end and he was whisked away to a higher place of additional monitoring.
Didnt have time to feel sad about having two very broken patients less than halfway through the shift as the man in bed 18 decided to pick that moment to go into a convincing supraventricular tachycardia with a rate of 160. He had no chest pain or shortness of breath, and no signs of shock so he wasnt compromised. Decided to try some valsalva manoeuvres with him (this raises intrathoracic pressure which activates the vagus nerve, and the parasympathetic stimulation in theory should slow the heart rate). Found myself pondering whether anybody else in the world was spending their time encouraging a 44 year old tachycardic to blow into a syringe at 4 am. Probably just me. Carotid massage didnt work either so called the med reg and we gave some adenosine. The underlying rhythm was atrial flutter, and as he hadnt spontaneously reverted to sinus rhythm the med reg sent him to the Coronary Care Unit.
To add to the fun I also had a 33 year old type 1 diabetic chap admitted with a sodium of 112 (very low) and a potassium of 5.4 (a little high). He was feeling dreadful, nauseus, dizzy on standing and we wondered if he might have Addison's disease (steroid deficiency). ECG showed peaked T waves so I treated his hyperkalaemia with IV calcium gluconate and insulin (with 50% dextrose) and he went hypo! Cue hypostop and more IV glucose.
Regarding his possible Addisons disease, his cortisol came back at 143 (lowish but not diagnostically so). We gave him some dexamethasone, a strong steroid that wouldnt affect the results of the Short Synacthen test (cortisol challenge test) in the morning. He also needed lying/standing blood pressures, an ACTH level and paired serum/urine osmolalities which I handed over to the day team.
I think I might be slightly in love with the med reg after last night. There's a good chance neither I nor the patients would have made it through last night without her!
Thursday, 1 December 2011
Dr Doctor - MAU Twilights
So the twilight shift entails coming into work around 2pm and working all the way through until 10. You dont look after a particular bay of patients, but instead float between all the bays helping out where needed.
Yesterday it seemed that every patient I went to was elderly, deaf and confused in equal measures. I felt bad that I had to take my histories at shouting volume, which afforded little privacy for the patients.
- HOW ARE YOUR BOWELS, SIR?
- THEY'RE STILL THERE DOCTOR! [cue endearing toothless grin]
It seems this week I have looking particularly youthful. I have had not one, but two nurses ask me if I'm a student. One of them I'm sure did it just to patronise me (unfortunately a fair few of the MAU nurses are lacking a degree of professional respect, which diminishes further if you dare to ask them to do their job). The tally of patients/relatives commenting on how young I look has risen to 24 in the past four months. They often compare me to their grandchildren. I'm getting used to the look of surprise when I introduce myself as one of the doctors.
Pretty harsh MAU shift pattern at the moment, 3 twilights, 1 day off then onto nights over the weekend. Somehow I'm working every weekend in December, including Christmas and my birthday. Social life destroyed. Morale low.
Yesterday it seemed that every patient I went to was elderly, deaf and confused in equal measures. I felt bad that I had to take my histories at shouting volume, which afforded little privacy for the patients.
- HOW ARE YOUR BOWELS, SIR?
- THEY'RE STILL THERE DOCTOR! [cue endearing toothless grin]
It seems this week I have looking particularly youthful. I have had not one, but two nurses ask me if I'm a student. One of them I'm sure did it just to patronise me (unfortunately a fair few of the MAU nurses are lacking a degree of professional respect, which diminishes further if you dare to ask them to do their job). The tally of patients/relatives commenting on how young I look has risen to 24 in the past four months. They often compare me to their grandchildren. I'm getting used to the look of surprise when I introduce myself as one of the doctors.
Pretty harsh MAU shift pattern at the moment, 3 twilights, 1 day off then onto nights over the weekend. Somehow I'm working every weekend in December, including Christmas and my birthday. Social life destroyed. Morale low.
Monday, 21 November 2011
Dr Doctor - MAU Days
Back to day shifts this week. Handover at 8am then the FY1 gets stuck in the MAU discharge lounge with the most stable patients that are waiting to go home. Left feeling demoted back to a secretarial role having completed 7 TTOs (discharge summaries) by lunchtime. BORED.
Sneak into Bay 1 to find a Stressed looking SHO juggling three sick patients with 3 others to be seen. Excellent! Patients with Stuff Wrong That Needs Sorting! Park myself in Bay 1 to relief of Stressed looking SHO. Clerk adorable elderly lady with COPD, possible infective exacerbation thereof but patient says she's not more SOB that usual (despite sats of 78% on admission and PO2 of 8 on the ABG), and doesnt have a productive cough. Spot a pleural effusion on the CXR (no recent weight loss/haemoptysis/sweats). Increased white cell count and CRP (inflammatory marker) but recent course of steroids (could raise WCC) Hmm. Consultant comes to review and is also unsure. Cover her with antibiotics for a chest infection (tablets EVERYWHERE!)
Bleeped back to the discharge lounge by nurses asking me to do stuff I've already done. Escape to the mess for a morale restoring cup of tea. Run into a second Stressed SHO running around Bay 3 and jump at chance to help her out. Offered choice between another possible pneumonia and a large PR bleed. Choose pneumonia.
Clerk adorable elderly gentleman with COPD, he's been more SOB than usual, and has a productive cough, sad to hear that the sputum has changed colour to "obviously pink" with some flecks of blood. He's lost 2 stone in weight over 6 months. Hmm. He was ex Navy, had smoked 40 a day for about 40 years, and kept telling me amusing stories about his life. Treat for COPD exacerbation, but suggest needs further investigation for underlying malignancy.
Handover at 8pm and back to hospital accommodation for something instantly cookable.
Sneak into Bay 1 to find a Stressed looking SHO juggling three sick patients with 3 others to be seen. Excellent! Patients with Stuff Wrong That Needs Sorting! Park myself in Bay 1 to relief of Stressed looking SHO. Clerk adorable elderly lady with COPD, possible infective exacerbation thereof but patient says she's not more SOB that usual (despite sats of 78% on admission and PO2 of 8 on the ABG), and doesnt have a productive cough. Spot a pleural effusion on the CXR (no recent weight loss/haemoptysis/sweats). Increased white cell count and CRP (inflammatory marker) but recent course of steroids (could raise WCC) Hmm. Consultant comes to review and is also unsure. Cover her with antibiotics for a chest infection (tablets EVERYWHERE!)
Bleeped back to the discharge lounge by nurses asking me to do stuff I've already done. Escape to the mess for a morale restoring cup of tea. Run into a second Stressed SHO running around Bay 3 and jump at chance to help her out. Offered choice between another possible pneumonia and a large PR bleed. Choose pneumonia.
Clerk adorable elderly gentleman with COPD, he's been more SOB than usual, and has a productive cough, sad to hear that the sputum has changed colour to "obviously pink" with some flecks of blood. He's lost 2 stone in weight over 6 months. Hmm. He was ex Navy, had smoked 40 a day for about 40 years, and kept telling me amusing stories about his life. Treat for COPD exacerbation, but suggest needs further investigation for underlying malignancy.
Handover at 8pm and back to hospital accommodation for something instantly cookable.
Saturday, 19 November 2011
Dr Doctor - MAU Nights 2
Currently spending the weekend recovering from MAU nights. At least I think it's the weekend, have been genuinely unsure of what day it is for some time now. Have decided one benefit of living on hospital grounds is the 30 second commute to work, but you do have to sleep through the noise of all the wailing ambulances during the day.
The last three nights have gone fairly well, with good variety of patients. Some of the most interesting included a gentleman in post renal renal failure with a urea of 50 and creatinine of 2550 (catheterise, IV fluids to match urine output plus 50mls to counteract post obstruction diuresis) whose creatinine had resolved to 250 by the end of the night. Another chap had come in via A&E with chest pain and been treated as an acute coronary syndrome despite no ECG changes. He was anaemic with a haemoglobin of 6.9 (further questioning revealed he had been GI bleeding for a couple of weeks) and actually had anaemia related myocardial ischaemia (stop antiplatelet meds and clexane, X match, transfuse, OGD).
The last night saw my bay turned into a secure unit - two known violent psych patients both admitted with shortness of breath, one from a forensic unit with two reassuringly large psych nurses guarding him was for male only nursing and doctoring due to his tendency to attack women. He was actually no trouble, but the other one caused issues demanding oxycodone in the middle of the night on top of his tramadol and co-codamol. Given that he had been admitted significantly hypoxic with a blood gas that showed a PO2 of 8 and type 2 respiratory failure I wasnt about to administer any more opiates no matter how loudly he yelled at me (because they can cause respiratory depression and oxycodone and tramadol are both quite strong anyway). The cynic in me wasnt convinced that he was truely in pain, or at least not the sort that would be aided by drugs - "where does it hurt sir?" "all over my body doctor" ..as he sat looking comfortable at rest.
The patient wasnt taking no for an answer from me so in the end I went to find the biggest SHO I could and got him to talk him down. Was quite reassured when he completely backed me up, explaining to the patient that I was doing the safe thing by not giving him the oxycodone and managed to calm him down.
Further 3am tutorials on liver disease from World's Most Enthusiastic Med Reg were made bearable by tea and cake, and we all made it through our final morning handover, me with three sick respiratory patients to present to a slightly grumpy highly seasoned respiratory consultant, and retired to bed delighted to have finished nights.
Labels:
ACS,
Anaemia,
Bed,
Handover,
Med Reg,
Nights,
Psych,
Renal Failure,
Respiratory Failure
Wednesday, 16 November 2011
Dr Doctor - MAU Nights
I have once again been thrown in at the deep end, starting my placement in MAU on nights. I'm currently unsure what day it is. Having never done nights before this was all very new. Main concern was how on earth I was going to manage to stay awake for 12 hours in the busiest department in the hospital and practise medicine to a reasonable standard on all the really quite unwell GP and A&E admissions.
Strategy for first night shift was to wake up mid morning, do lots of exercise to knacker myself out and then sleep for a few hours in the afternoon.
8pm handover resulted in me being assigned an entire bay of 10 patients to look after, and to clerk, treat and triage any new admissions to that bay. I also got handed an SHO bleep, and a crash bleep.
Patients in my bay included a paracetamol overdose (check levels, continue acetylcysteine), a young diabetic ketoacidosis (repeat blood gas, monitor blood glucose, continue fluids and insulin), a seizure ?cause (check bloods, arrange urgent CT and report), 2 young patients with severe community acquired pneumonia (for IV antibiotics), a tall thin young man with a pneumothorax (chest drain in situ) and one chap with terminal cholangiocarcinoma presenting with gastric outflow obstruction, vomiting and hypovolaemic shock (arrange erect CXR and AXR, NG tube on free drainage, antiemetics, fluid resuscitation, keep seniors well informed).
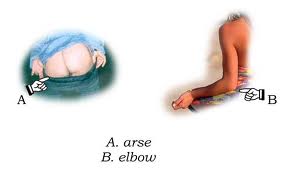
We also had three confused gentlemen, one of whom escaped from his bed around 2 am and, gown flapping the breeze, buttocks defiantly on show to the ward, pulled back the curtains of his neighbour and proceeded to relieve himself thankfully beside his bed and not onto him! "OI!! He's pissing at me! Bastard! NURSE!"
Around 3pm our bright eyed and enthusiastic Med Reg insisted on giving all the juniors a formal powerpoint tutorial on upper GI bleeding. Thought it was a nice touch that he made us all a big pot of tea to drink while we sat and tried to stay awake while he talked about the most recent papers in the field.
Around 6am the crash bleep went off so the Med Reg and I ran across the hospital and up three flights of stairs to find a proper cardiac arrest in full swing on one of the surgical wards. I joined in with chest compressions. The patient was in VF and was shocked 5 times before going into asystole. Resus continued and somehow he went back into sinus rhythm with an output. This was short lived however as he then went into VT. 7 shocks, many antiarrhythmics and some potassium later his heart decided to stay in sinus rhythm and the patient went to ITU. Apparently an echo showed a massive ventricular aneurysm, probably secondary to a huge heart attack, so sadly he probably wont recover from this.
8am handover involved presenting the sickest patients to the day team and then home to bed. All in all a good first night.
Strategy for first night shift was to wake up mid morning, do lots of exercise to knacker myself out and then sleep for a few hours in the afternoon.
8pm handover resulted in me being assigned an entire bay of 10 patients to look after, and to clerk, treat and triage any new admissions to that bay. I also got handed an SHO bleep, and a crash bleep.
Patients in my bay included a paracetamol overdose (check levels, continue acetylcysteine), a young diabetic ketoacidosis (repeat blood gas, monitor blood glucose, continue fluids and insulin), a seizure ?cause (check bloods, arrange urgent CT and report), 2 young patients with severe community acquired pneumonia (for IV antibiotics), a tall thin young man with a pneumothorax (chest drain in situ) and one chap with terminal cholangiocarcinoma presenting with gastric outflow obstruction, vomiting and hypovolaemic shock (arrange erect CXR and AXR, NG tube on free drainage, antiemetics, fluid resuscitation, keep seniors well informed).
We also had three confused gentlemen, one of whom escaped from his bed around 2 am and, gown flapping the breeze, buttocks defiantly on show to the ward, pulled back the curtains of his neighbour and proceeded to relieve himself thankfully beside his bed and not onto him! "OI!! He's pissing at me! Bastard! NURSE!"
Around 3pm our bright eyed and enthusiastic Med Reg insisted on giving all the juniors a formal powerpoint tutorial on upper GI bleeding. Thought it was a nice touch that he made us all a big pot of tea to drink while we sat and tried to stay awake while he talked about the most recent papers in the field.
Around 6am the crash bleep went off so the Med Reg and I ran across the hospital and up three flights of stairs to find a proper cardiac arrest in full swing on one of the surgical wards. I joined in with chest compressions. The patient was in VF and was shocked 5 times before going into asystole. Resus continued and somehow he went back into sinus rhythm with an output. This was short lived however as he then went into VT. 7 shocks, many antiarrhythmics and some potassium later his heart decided to stay in sinus rhythm and the patient went to ITU. Apparently an echo showed a massive ventricular aneurysm, probably secondary to a huge heart attack, so sadly he probably wont recover from this.
8am handover involved presenting the sickest patients to the day team and then home to bed. All in all a good first night.
Friday, 11 November 2011
Dr Doctor your ear!
Was amused by the following exchange between one of our more deaf patients, and a nurse:
- Hello Leonard! I've got your hearing aid, can I put it in your ear?
- My rear? No you may not!
- Your ear, Leonard, YOUR EAR
- Yes, I know I'm here. Now what do you want?
Friday, 28 October 2011
Dr Doctor can you pull the curtains back?
Some of our patients really are hilarious. Yesterday evening I was taking blood from one gentleman, when the chap in the next bed (which was surrounded by curtains) farted extremely loudly to himself and said "Sorry about that" presumably to the rest of us in the room. When I had finished taking blood I went to leave, and as I walked past the other chap's bed he said "Oh doctor, could you pull the curtains back please?" I drew back the curtains to reveal a middle aged man, spreadeagled on his bed, stark bollock naked with a massive grin on his face and waving at me. Unsurprisingly I pulled the curtains around again!
Had a bleep from a rather stressed SHO on the winter overflow ward to ask me to take blood:
- I'm really sorry, it's just that I was supposed to finish an hour ago and this man needs an INR taking but he's shat all over himself, and the bed, and the floor, would you mind doing it for me?
- Er.. I think I'll wait half an hour for him to be cleaned up, but yes that's fine!
Arrived half an hour later to take the blood to find an innocuous looking (clean) elderly man. First thought - "well you dont look like the type to have recently been entirely covered in faeces". Second thought - "I'm NOT kneeling on the floor".
Pulled the curtains round the bed and started taking blood, when the patient in the next bed started vomiting profusely, much to the dismay of his visiting relatives.
- Bleurgh BLEEUUUUURGH Oh God it's the soup! BLEUUURGH.
Thursday, 27 October 2011
Dr Doctor my bleep's exploded!
Entered the doctors mess yesterday evening to find two fellow FY1s in state of panic clustered round the coffee table. There was the sound of a slightly forlorn pager tone mixed in with cries of:
- Quick get it out, get it out!
- I cant get the back off!
- Ow it's really hot!
I joined the commotion to find one of them attacking a pager with a butter knife, apparently trying to prise the battery out of it. The bleep was bleeping continuously in a very odd tone and smoke appeared to be rising from it. My colleague succeeded in prising the back off to reveal a rather melty looking battery! She looked somewhat tearfully at it and said "This is the SAU on call bleep, it hasnt stopped going off all evening and then it got really hot and started smoking! And it made this weird noise and I thought it was going to explode." So this is what I have to look forward to when I get to the surgical admissions unit.
- Quick get it out, get it out!
- I cant get the back off!
- Ow it's really hot!
I joined the commotion to find one of them attacking a pager with a butter knife, apparently trying to prise the battery out of it. The bleep was bleeping continuously in a very odd tone and smoke appeared to be rising from it. My colleague succeeded in prising the back off to reveal a rather melty looking battery! She looked somewhat tearfully at it and said "This is the SAU on call bleep, it hasnt stopped going off all evening and then it got really hot and started smoking! And it made this weird noise and I thought it was going to explode." So this is what I have to look forward to when I get to the surgical admissions unit.
Tuesday, 25 October 2011
Dr Doctor with pulmonary oedema.
The rest of yesterday's on call shift went rather well. I was called to see a patient I had treated for pulmonary oedema on Friday when he was admitted. He had had a stroke and a proper swallow assessment hadnt been done so he had been made nil by mouth and not received any of his oral medication to stop him going into heart failure again over the weekend, so he promptly went back into heart failure and was feeling awful. It would have been helpful if one of the nurses doing the drugs round had alerted a doctor that he couldnt take his meds.
I examined him and wrote up the same treatment he had had on Friday - 40mg IV Furosemide and 2.5mg IV diamorphine. I repeated the CXR and did an ABG. He was quite tachycardic and said he had chest pain so did an ECG. Asked nurses to do hourly obs and monitor fluid input/output.
I was slightly concerned this chap might also have a pulmonary embolism as the ECG showed sinus tachycardia, the chest pain sounded pleuritic (worse on taking a deep breath), his ABG had a very low PaO2 [7.6 EEK increase the oxygen!] and I found a tender right calf on examination. Quite difficult to know what to do about this as therapeutic dose clexane is contraindicated with a large ischaemic stroke as it carries a high risk of bleeding. He probably wasnt a candidate for inferior vena caval filters (to prevent a thrombus travelling from a DVT in the leg to the lungs).
Decided to discuss with the med reg, who came to see the patient. She suggested starting a GTN infusion because the patient's blood pressure was stable at 150 systolic (GTN is likely to drop the BP considerably so should be started with caution.) She also said well done, which gave me some reassurance that I do have a vague idea about what I'm supposed to be doing!
Dr Doctor - a toilet emergency.
So some smart electrician has switched the emergency toilet alarm with the light. We only discovered this after the third little old person was found looking more dazed and confused than usual but otherwise perfectly fine in the doorway to the toilet, blinking at the large crowd of nurses and doctors that had descended en mass when the alarms went off. After the third time the response was a little slower to the fourth, and we arrived to find a little old man floundering on his back on the floor having fallen over in surprise when the alarms went off!
Saturday, 22 October 2011
Dr Doctor is it because of my mum?
Interesting consultation with a patient who had had a stroke this week:
- So do you understand that the scan results show that you've had a stroke?
- Yes doctor, I understand that, I just dont understand why it happened.
- Well, you've had high blood pressure for a long time, you have an irregular heart beat and have been smoking 40 cigarettes a day for 40 years, all these things have probably contributed.
- Alright, but was it anything to do with my mother?
- Your mother? Did she have a stroke?
- No, she had a pacemaker.
- I see. Well sometimes things like high cholesterol can run in families and that can increase your risk of a stroke.
- Hmm. So will I get it then?
- High cholesterol? At the moment your cholesterol is within normal limits.
- No, my mother's pacemaker. Is that inherited?
- Not unless she left it in her will..
- So do you understand that the scan results show that you've had a stroke?
- Yes doctor, I understand that, I just dont understand why it happened.
- Well, you've had high blood pressure for a long time, you have an irregular heart beat and have been smoking 40 cigarettes a day for 40 years, all these things have probably contributed.
- Alright, but was it anything to do with my mother?
- Your mother? Did she have a stroke?
- No, she had a pacemaker.
- I see. Well sometimes things like high cholesterol can run in families and that can increase your risk of a stroke.
- Hmm. So will I get it then?
- High cholesterol? At the moment your cholesterol is within normal limits.
- No, my mother's pacemaker. Is that inherited?
- Not unless she left it in her will..
Tuesday, 18 October 2011
Dr Doctor - a postural drop of 140!
Really interesting case on the ward at the moment. 80 year old man admitted with TIA type symptoms whenever he stood up. Found to have a postural drop in systolic blood pressure between 90 - 140 mmHg. Just to put that in perspective, postural hypotension is considered to be a drop in systolic BP of more than 15 mmHg. The usual culprit is too many antihypertensive medications.
Trouble with this chap is, his systolic BP usually runs around 200 (normal is around 120). Treatment for postural hypotension (after stopping antihypertensive meds) is fludrocortisone, a potent steroid that acts like aldosterone to increase sodium and water retention. Contraindicated in this chap with such a high systolic BP.
The team is also somewhat baffled by the cause of this phenomenon. Addison's disease is a possibility, but random cortisol measurement was normal, suggesting he doesnt have a steroid deficiency. He doesnt have diabetes, so autonomic neuropathy is unlikely, although there are a few other rare causes of autonomic neuropathy. He doesnt have Parkinson's disease so this cant be multisystem atrophy (a Parkinson's plus syndrome affecting the autonomic nervous system). Maybe he has some sort of baroreceptor problem.
We're also unsure as to why his usual systolic BP is so high, and are considering secondary causes of hypertension. He does have chronic kidney disease (renal artery stenosis or other intrinsic renal disease could cause raised BP). We're awaiting 24 hour catecholamine levels (if raised may indicate a phaeochromocytoma - rare adrenaline secreting tumour). We should check his other hormones for Cushing's, Conn's and acromegaly, and look for coarctation of the aorta.
Oh dear, I seem to have regurgitated a medical textbook.
Trouble with this chap is, his systolic BP usually runs around 200 (normal is around 120). Treatment for postural hypotension (after stopping antihypertensive meds) is fludrocortisone, a potent steroid that acts like aldosterone to increase sodium and water retention. Contraindicated in this chap with such a high systolic BP.
The team is also somewhat baffled by the cause of this phenomenon. Addison's disease is a possibility, but random cortisol measurement was normal, suggesting he doesnt have a steroid deficiency. He doesnt have diabetes, so autonomic neuropathy is unlikely, although there are a few other rare causes of autonomic neuropathy. He doesnt have Parkinson's disease so this cant be multisystem atrophy (a Parkinson's plus syndrome affecting the autonomic nervous system). Maybe he has some sort of baroreceptor problem.
We're also unsure as to why his usual systolic BP is so high, and are considering secondary causes of hypertension. He does have chronic kidney disease (renal artery stenosis or other intrinsic renal disease could cause raised BP). We're awaiting 24 hour catecholamine levels (if raised may indicate a phaeochromocytoma - rare adrenaline secreting tumour). We should check his other hormones for Cushing's, Conn's and acromegaly, and look for coarctation of the aorta.
Oh dear, I seem to have regurgitated a medical textbook.
Sunday, 16 October 2011
Dr Doctor - should I say something?
I'll never forget one of my endocrinology lecturers in medical school professing about how he had diagnosed the lady in his local fish and chip shop with acromegaly the first day he laid eyes on her, and that every time he went for his cod and chips wrestled with the dilemma as to whether or not he should tell her his diagnosis.
- I'll have the large cod and chips thanks, no peas, by the way, you know that huge nose of yours, the masculine brow and all that facial hair? yeah well, I reckon you've got acromegaly.
- I beg your pardon!? acrowhat? how DARE you!
- Well it was merely an observation madam, that you have been looking increasingly like a man over the years, and I think I know the reason - you've got a pituitary tumour. [nods smugly]
- A what?
- A tumour, in part of your brain, secreting growth hormone. That's why your hands are like spades and your shoe size has increased 10 sizes in the past five years.
- So you're telling me I look like a man and I have a brain tumour??
- Yes it's probably the reason you sweat so much and your skin is so greasy. You need to see an endocrinologist, and it's your lucky day..!
I suspect he probably still hasnt broached the subject. I had a similar dilemma myself the other day when I noticed that the bank clerk sorting out my friend's accounts had stage 3 finger clubbing. He was a young guy, around late 20s, looked fairly healthy. What was I to do? It could be normal for him, or he could have some serious underlying disease. I spent a good 20 minutes staring at this chap's fingers, he must have thought I was rather odd. But what could I do? It didnt seem the time or the place to bring the subject up.
Did I have a duty of care to this guy simply because I am a doctor and my level of knowledge allows me to recognise such a clinical sign as being potentially significant? If I was his GP and he were sat in my consulting room I would have no issue with asking him reams of intimate questions in an attempt to screen for any potential serious disease but with roles reversed, such a course of action seemed most inappropriate.
Perhaps I could have asked how long his fingernails has been like that. My most likely differential was something like cystic fibrosis or crohn's disease, which if he had, he would know about and would probably know his fingers were clubbed. This would then be easy, he could smile knowingly and say "a very long time" and I could smile knowingly and say "I'm a doctor, couldnt help but notice" and leave it at that. The problem would come if he had no idea there was anything wrong with his fingernails, as bringing it up then carried a high risk of either causing offence or inciting great terror, or both.
- How long have your fingernails been like that?
- My fingernails? What's wrong with my fingernails?
- Well, they're clubbed, it could be a sign of serious underlying disease. Or it could be nothing.
- What sort of underlying disease?
- Oh many things, lung cancer, TB, bacterial endocarditis, cirrhosis.. how are your bowels?
- Pardon?
- I said how are your BOWELS? [other bank customers turn round to look]
- They're fine.
- Probably not crohn's disease or ulcerative colitis then. Hmm, you do look a bit syndromic, could be congenital cyanotic heart disease.
Hmm.. probably a good thing I didn't say anything, but I am curious.
- I'll have the large cod and chips thanks, no peas, by the way, you know that huge nose of yours, the masculine brow and all that facial hair? yeah well, I reckon you've got acromegaly.
- I beg your pardon!? acrowhat? how DARE you!
- Well it was merely an observation madam, that you have been looking increasingly like a man over the years, and I think I know the reason - you've got a pituitary tumour. [nods smugly]
- A what?
- A tumour, in part of your brain, secreting growth hormone. That's why your hands are like spades and your shoe size has increased 10 sizes in the past five years.
- So you're telling me I look like a man and I have a brain tumour??
- Yes it's probably the reason you sweat so much and your skin is so greasy. You need to see an endocrinologist, and it's your lucky day..!
I suspect he probably still hasnt broached the subject. I had a similar dilemma myself the other day when I noticed that the bank clerk sorting out my friend's accounts had stage 3 finger clubbing. He was a young guy, around late 20s, looked fairly healthy. What was I to do? It could be normal for him, or he could have some serious underlying disease. I spent a good 20 minutes staring at this chap's fingers, he must have thought I was rather odd. But what could I do? It didnt seem the time or the place to bring the subject up.
Did I have a duty of care to this guy simply because I am a doctor and my level of knowledge allows me to recognise such a clinical sign as being potentially significant? If I was his GP and he were sat in my consulting room I would have no issue with asking him reams of intimate questions in an attempt to screen for any potential serious disease but with roles reversed, such a course of action seemed most inappropriate.
Perhaps I could have asked how long his fingernails has been like that. My most likely differential was something like cystic fibrosis or crohn's disease, which if he had, he would know about and would probably know his fingers were clubbed. This would then be easy, he could smile knowingly and say "a very long time" and I could smile knowingly and say "I'm a doctor, couldnt help but notice" and leave it at that. The problem would come if he had no idea there was anything wrong with his fingernails, as bringing it up then carried a high risk of either causing offence or inciting great terror, or both.
- How long have your fingernails been like that?
- My fingernails? What's wrong with my fingernails?
- Well, they're clubbed, it could be a sign of serious underlying disease. Or it could be nothing.
- What sort of underlying disease?
- Oh many things, lung cancer, TB, bacterial endocarditis, cirrhosis.. how are your bowels?
- Pardon?
- I said how are your BOWELS? [other bank customers turn round to look]
- They're fine.
- Probably not crohn's disease or ulcerative colitis then. Hmm, you do look a bit syndromic, could be congenital cyanotic heart disease.
Hmm.. probably a good thing I didn't say anything, but I am curious.
Saturday, 15 October 2011
Dr Doctor - A Day of Incompetence
I had "one of those days" the other day. Almost everything I did seemed to be wrong in some way, and I made a catalogue of (thankfully mostly minor) Mistakes. Now doctors aren't supposed to make Mistakes, we're invincible. And when we do make Mistakes we're not supposed to talk about them because we're just that egotistical. There have been various headlines in the recent press about the instant dismissal of whistleblowers (the people who have seen something wrong and tried to put it right in an effort to improve patient care, affronted a few people's egos and been booted out the door). The airline industry had similar problems a good many years ago and have since invested in Crew Resource Management Training to break down the barriers of hierarchy and allow more junior staff to speak up if they see a problem. Mistakes are considered learning opportunities in a culture that lacks blame. The only part of medicine that has a similar attitude to patient safety is anaesthetics.
So I will tell you about my day, and my Mistakes, because maybe somebody else will get to learn from them, and patient care will ultimately be improved.
The day began with the most ferocious of medical registrars (who also happened to be post nights) striding onto the ward and barking at me that I was on call and therefore should have been at handover while brandishing the on-call bleep at me. I genuinely hadnt realised I was on call, so naturally hadnt turned up. I apologised and willingly took the bleep, hoping that this wouldnt set the tone for my day.
A few hours later, my consultant came to find me, carrying possibly the first TTO (To Take Out - a discharge summary with the patient's discharge medications and further instructions for the GP for continuing care) I had ever written, back when I had no idea what a TTO really was and what meds the patients needed. He gently pointed out that I had failed to write down that the GP needed to start Clopidogrel 75mg after 2 weeks of 300mg Aspirin, which meant that this post stroke patient had had no antiplatelet medication for about 3 weeks. Had this patient had another stroke in this time it could have been my fault. Thankfully they hadn't, but I felt really bad at having made a potentially serious Mistake. The TTOs are screened by a pharmacist before the patient is discharged, so it should have been picked up by pharmacy (note it usually takes more than one mistake to lead to an adverse incident - google Swiss Cheese Model of System Failure). I was glad my consultant had pointed this out (although by now I'd been doing TTOs correctly for quite some time) but what did make me somewhat miffed was our slightly pushy pharmacist (she's the type of person who enjoys bossing others around) butting in, immediately defending herself that it wasn't her that checked this TTO, and turning round to me and in front of my consultant saying "Oh yes, well you remember we had that talk about prescribing medications after discharge." This made it sound as if I had a problem with my prescribing and made me look pretty crap in front of my consultant. In actual fact we had had no such conversation, but she had yelled at me a couple of weeks ago for accidentally signing off an electronic discharge summary before she had seen it. I thanked my consultant, assured him it wouldnt happen again, and left.
Next, I was accosted by the end of life team nurse while ward rounding with another consultant. She wanted to know if I had spoken to a patient's family about deciding whether or not to palliate her. Now, generally I would expect this to be a consultant led conversation, given that end of life decisions are consultant decisions and out of respect for the patient and their family. The nurse had assumed that because I had documented "Discuss with family regards palliation" on behalf of the consultant on yesterday's ward round that I had made the decision and therefore I should have done it. The plan had not been handed over to the afternoon consultant by the morning consultant so neither of them had spoken to the family, and I ended up looking bad again. I probably should have made sure the afternoon consultant was aware of the plan, but things are easily missed when we're all so busy with other jobs.
So I spent the day feeling rather incompetent, but at least it's given me a lot of things to write in the "reflective practise" section of my e-portfolio! I'm well aware that if these are the worst Mistakes I ever make, I will actually be doing rather well.
So I will tell you about my day, and my Mistakes, because maybe somebody else will get to learn from them, and patient care will ultimately be improved.
The day began with the most ferocious of medical registrars (who also happened to be post nights) striding onto the ward and barking at me that I was on call and therefore should have been at handover while brandishing the on-call bleep at me. I genuinely hadnt realised I was on call, so naturally hadnt turned up. I apologised and willingly took the bleep, hoping that this wouldnt set the tone for my day.
A few hours later, my consultant came to find me, carrying possibly the first TTO (To Take Out - a discharge summary with the patient's discharge medications and further instructions for the GP for continuing care) I had ever written, back when I had no idea what a TTO really was and what meds the patients needed. He gently pointed out that I had failed to write down that the GP needed to start Clopidogrel 75mg after 2 weeks of 300mg Aspirin, which meant that this post stroke patient had had no antiplatelet medication for about 3 weeks. Had this patient had another stroke in this time it could have been my fault. Thankfully they hadn't, but I felt really bad at having made a potentially serious Mistake. The TTOs are screened by a pharmacist before the patient is discharged, so it should have been picked up by pharmacy (note it usually takes more than one mistake to lead to an adverse incident - google Swiss Cheese Model of System Failure). I was glad my consultant had pointed this out (although by now I'd been doing TTOs correctly for quite some time) but what did make me somewhat miffed was our slightly pushy pharmacist (she's the type of person who enjoys bossing others around) butting in, immediately defending herself that it wasn't her that checked this TTO, and turning round to me and in front of my consultant saying "Oh yes, well you remember we had that talk about prescribing medications after discharge." This made it sound as if I had a problem with my prescribing and made me look pretty crap in front of my consultant. In actual fact we had had no such conversation, but she had yelled at me a couple of weeks ago for accidentally signing off an electronic discharge summary before she had seen it. I thanked my consultant, assured him it wouldnt happen again, and left.
Next, I was accosted by the end of life team nurse while ward rounding with another consultant. She wanted to know if I had spoken to a patient's family about deciding whether or not to palliate her. Now, generally I would expect this to be a consultant led conversation, given that end of life decisions are consultant decisions and out of respect for the patient and their family. The nurse had assumed that because I had documented "Discuss with family regards palliation" on behalf of the consultant on yesterday's ward round that I had made the decision and therefore I should have done it. The plan had not been handed over to the afternoon consultant by the morning consultant so neither of them had spoken to the family, and I ended up looking bad again. I probably should have made sure the afternoon consultant was aware of the plan, but things are easily missed when we're all so busy with other jobs.
So I spent the day feeling rather incompetent, but at least it's given me a lot of things to write in the "reflective practise" section of my e-portfolio! I'm well aware that if these are the worst Mistakes I ever make, I will actually be doing rather well.
Thursday, 6 October 2011
Dr Doctor the BP is 60/40!
Yesterday I was called to see an 89 year old patient with a blood pressure of 60/40 (my heart rate picked up when I heard this). Details from the nurse on the phone - the rest of the obs were stable, except the sats probe wasnt picking up a reading (this worried me because it might mean the patient is so peripherally shut down that it's not picking up a reading. Patient had been admitted with sepsis (with a resultant acute kidney injury), probably due to her bilateral cellulitis, and was on the appropriate antibiotics for this. Past medical history of note included end stage congestive cardiac failure - this complicates matters when considering fluid resuscitation because if I think she's dehydrated and give her fluids too quickly I could overload her and precipitate massive pulmonary oedema which could be the end of her.
Took stairs two at a time to the ward. Patient looked unwell and SOB (short of breath), and was quite drowsy and confused (not a good sign). On examination she was very peripherally cool, with a peripheral capillary refill time of more than 6 seconds (heart sank a little at this point) central cap refill was 3-4 seconds (hmm, still longer than it should be). Heart sounds were normal, but I discovered she had bilateral crackles throughout both lungs (did she have a chest infection or was this pulmonary oedema?). As all previous chest examinations in the notes had said chest was clear I decided to repeat a chest xray (CXR). Her previous CXR from the day before showed signs of heart failure with no obvious consolidation. The rest of the examination was unremarkable. Managed to make sats probe work for a short period which showed her sats were 98% on 2L oxygen so reassured. Noted patient was already catheterised (important to allow montoring of urine output). Started 24hour bag of fluids, encouraged patient to drink (water, although we could have both probably benefitted from a brandy at this point!), with a view to having a senior review regarding IV fluids.
I decided to check her latest blood results which showed a low sodium 120 and a high potassium 5.9. Asked the nurses to do an ECG (no new changes). Checked her drug chart - she was on spironolactone which could account for the abnormal electrolytes, but with end stage heart failure there was no way I was going to stop this and would need to discuss it with a senior in any case. Also noticed she was on an ACE inhibitor so stopped this with day team to review as this may have been contributing to her renal failure.
Also on the system was a urine culture that was positive for klebsiella that she was not being treated for. Started trimethoprim (having checked the BNF regarding dosage regimen in renal failure).
Decided to repeat a full set of bloods and do an ABG (would be discussing patient with some sort of med reg who would be highly likely to want to know the results of this). Ordered CXR, instructed nurses to do hourly obs and monitor hourly input/output and ran the case past my SHO.
Went back to review the patient a couple of hours later, she hadnt deteriorated and her blood pressure was slightly better. Her CXR showed no focal consolidation (so probably not a chest infection) and worsening signs of heart failure.
Presented all of the above to the senior night team at 10pm handover (included the fact she was DNAR and her past history), and must have placated the previously disgruntled cardiology registrar who said that was a much better handover than the previous night. Gained a sense of achievement for a productive evening's work.
Took stairs two at a time to the ward. Patient looked unwell and SOB (short of breath), and was quite drowsy and confused (not a good sign). On examination she was very peripherally cool, with a peripheral capillary refill time of more than 6 seconds (heart sank a little at this point) central cap refill was 3-4 seconds (hmm, still longer than it should be). Heart sounds were normal, but I discovered she had bilateral crackles throughout both lungs (did she have a chest infection or was this pulmonary oedema?). As all previous chest examinations in the notes had said chest was clear I decided to repeat a chest xray (CXR). Her previous CXR from the day before showed signs of heart failure with no obvious consolidation. The rest of the examination was unremarkable. Managed to make sats probe work for a short period which showed her sats were 98% on 2L oxygen so reassured. Noted patient was already catheterised (important to allow montoring of urine output). Started 24hour bag of fluids, encouraged patient to drink (water, although we could have both probably benefitted from a brandy at this point!), with a view to having a senior review regarding IV fluids.
I decided to check her latest blood results which showed a low sodium 120 and a high potassium 5.9. Asked the nurses to do an ECG (no new changes). Checked her drug chart - she was on spironolactone which could account for the abnormal electrolytes, but with end stage heart failure there was no way I was going to stop this and would need to discuss it with a senior in any case. Also noticed she was on an ACE inhibitor so stopped this with day team to review as this may have been contributing to her renal failure.
Also on the system was a urine culture that was positive for klebsiella that she was not being treated for. Started trimethoprim (having checked the BNF regarding dosage regimen in renal failure).
Decided to repeat a full set of bloods and do an ABG (would be discussing patient with some sort of med reg who would be highly likely to want to know the results of this). Ordered CXR, instructed nurses to do hourly obs and monitor hourly input/output and ran the case past my SHO.
Went back to review the patient a couple of hours later, she hadnt deteriorated and her blood pressure was slightly better. Her CXR showed no focal consolidation (so probably not a chest infection) and worsening signs of heart failure.
Presented all of the above to the senior night team at 10pm handover (included the fact she was DNAR and her past history), and must have placated the previously disgruntled cardiology registrar who said that was a much better handover than the previous night. Gained a sense of achievement for a productive evening's work.
Tuesday, 4 October 2011
Dr Doctor on call again.
Late shifts on call again this week, and the last two have been a combination of marathon running, fire fighting, patient bleeding, nurse dodging and cardiology registrar disgruntling.
Number of bleeps - innumerable.
Number of flights of stairs traversed at speed - 20
Number of patients spiking temperatures requiring septic screens - 8
Number of times had to run to a different ward to find equipment for taking blood cultures - 4
Number of bloods needing checking according to afternoon handover - 12
Number of bloods handed to me to do by slightly slacking SHO - 3
Number of deranged U&E results requiring action - 2
Number of INR needing checked and warfarin prescribing - 5
Number of bloods needing repeating due to underfilled/haemolysed/lost/mislabelled - 3
Number of cannulas inserted - 3
Number of radiological investigations needing review - 5
Number of patients falling off their perches - 3
Number of times accosted by marauding nurses brandishing drugs charts/incomplete sets of obs - 7
Number of minutes spent in doctors' mess inhaling sandwich and cup of tea - 15
Number of minutes spent regretting such indulgence - 0 (no time!)
Helpfully, one patient decided to fall off their perch around 9pm, 1 hour before handover to the night team. They needed to be examined, septic screened (bloods, blood cultures, CXR, urine dip, microscopy&culture), writing up for antibiotics based on my examination findings (focus of infection probably chest), a cannula inserting and fluids prescribing, handover to nursing staff and handover at handover. In my haste to get on and determine that he was septic and instigate the septic screen and some treatment before handover I didnt have time to look through the notes to determine why he was in hospital or his past medical history or whether he was for resus. My handover to the night SHO as a result was somewhat incomplete, which drew much criticism from the night cardiology registrar (cleverly masked behind the phrase "I'm not criticising..") and much cringing from me who should have done better.
Number of bleeps - innumerable.
Number of flights of stairs traversed at speed - 20
Number of patients spiking temperatures requiring septic screens - 8
Number of times had to run to a different ward to find equipment for taking blood cultures - 4
Number of bloods needing checking according to afternoon handover - 12
Number of bloods handed to me to do by slightly slacking SHO - 3
Number of deranged U&E results requiring action - 2
Number of INR needing checked and warfarin prescribing - 5
Number of bloods needing repeating due to underfilled/haemolysed/lost/mislabelled - 3
Number of cannulas inserted - 3
Number of radiological investigations needing review - 5
Number of patients falling off their perches - 3
Number of times accosted by marauding nurses brandishing drugs charts/incomplete sets of obs - 7
Number of minutes spent in doctors' mess inhaling sandwich and cup of tea - 15
Number of minutes spent regretting such indulgence - 0 (no time!)
Helpfully, one patient decided to fall off their perch around 9pm, 1 hour before handover to the night team. They needed to be examined, septic screened (bloods, blood cultures, CXR, urine dip, microscopy&culture), writing up for antibiotics based on my examination findings (focus of infection probably chest), a cannula inserting and fluids prescribing, handover to nursing staff and handover at handover. In my haste to get on and determine that he was septic and instigate the septic screen and some treatment before handover I didnt have time to look through the notes to determine why he was in hospital or his past medical history or whether he was for resus. My handover to the night SHO as a result was somewhat incomplete, which drew much criticism from the night cardiology registrar (cleverly masked behind the phrase "I'm not criticising..") and much cringing from me who should have done better.
Thursday, 29 September 2011
Dr Doctor, what was that about an enema?
Had a discussion with my SHO today about one of our dear old patients with dementia who frequently and loudly calls out the word "OW-OO" when awake, as if she might be in pain. Daily attempts to discover any potential source of pain have been unsuccessful, and the numerous pain medications she's taking are merely making her drowsy.
-Yeah, her abdominal x-ray showed that she's constipated up to the eyeballs.
- Are we giving her stuff for that?
- Oh yes, she's had suppositories and things.
- Could we not give her an enema?
- People who have enemas tend to explode themselves.
- I'm sorry?
- Yeah we had one lady who was bunged up like this so we gave her three enemas in one day and she exploded EVERYWHERE and then couldn't stop and gave herself an acute kidney injury because she'd dried herself out. She nearly died.
- Well that would be a crap way to go..
On another note, syphilis is on the rise again. I learned today that syphilis serology is part of the routine dementia blood screen in this Trust. I also learned that it is one of those samples that needs to get to the lab very soon after it has been taken (this entails a lot of fast walking as the pod system is not quick enough or reliable enough to be trusted). Most tests for hormone levels are the same (except cortisol, which is very stable) and lab technicians insist that a lactate sample needs to arrive instantaneously for fear of degredation (although I did hear a seasoned haematologist disputing this fact at great length the other day).
One of today's numerous trips to the lab involved me pitching up at the hatch, brandishing several samples and saying something along the lines of "I've got syphilis, vitamin D, a PTH, a stool sample and a blood gas." The grumpy bearded lab technician raised an eyebrow and muttered "Everyone's got bloody syphilis these days.."
I waited for the blood gas results, which were rather interesting. All the values were normal, except the PaO2 (arterial oxygen level) which was 23.7. Now if you know what I'm talking about you'll be thinking that the patient is clearly on supplemental oxygen, as normal PaO2 is around 13, and the partial pressure of oxygen in room air is 21 (21% oxygen in air) but nope, patient was on room air, and had a suspected pulmonary embolus so the PO2 should have been low..
I was a little stumped, until I figured out that the sample must have had an air bubble in it which affected the result. Although, this must mean that the stroke unit is an exceptionally oxygen rich environment as 23.7 is higher than the norm.
-Yeah, her abdominal x-ray showed that she's constipated up to the eyeballs.
- Are we giving her stuff for that?
- Oh yes, she's had suppositories and things.
- Could we not give her an enema?
- People who have enemas tend to explode themselves.
- I'm sorry?
- Yeah we had one lady who was bunged up like this so we gave her three enemas in one day and she exploded EVERYWHERE and then couldn't stop and gave herself an acute kidney injury because she'd dried herself out. She nearly died.
- Well that would be a crap way to go..
On another note, syphilis is on the rise again. I learned today that syphilis serology is part of the routine dementia blood screen in this Trust. I also learned that it is one of those samples that needs to get to the lab very soon after it has been taken (this entails a lot of fast walking as the pod system is not quick enough or reliable enough to be trusted). Most tests for hormone levels are the same (except cortisol, which is very stable) and lab technicians insist that a lactate sample needs to arrive instantaneously for fear of degredation (although I did hear a seasoned haematologist disputing this fact at great length the other day).
One of today's numerous trips to the lab involved me pitching up at the hatch, brandishing several samples and saying something along the lines of "I've got syphilis, vitamin D, a PTH, a stool sample and a blood gas." The grumpy bearded lab technician raised an eyebrow and muttered "Everyone's got bloody syphilis these days.."
I waited for the blood gas results, which were rather interesting. All the values were normal, except the PaO2 (arterial oxygen level) which was 23.7. Now if you know what I'm talking about you'll be thinking that the patient is clearly on supplemental oxygen, as normal PaO2 is around 13, and the partial pressure of oxygen in room air is 21 (21% oxygen in air) but nope, patient was on room air, and had a suspected pulmonary embolus so the PO2 should have been low..
I was a little stumped, until I figured out that the sample must have had an air bubble in it which affected the result. Although, this must mean that the stroke unit is an exceptionally oxygen rich environment as 23.7 is higher than the norm.
Wednesday, 28 September 2011
Dr Doctor it's like being in prison..
I heard one of the consultants discussing how being in hospital is actually rather like being in prison. We trap patients in a room with other sick people and wont let them leave, take away their clothes and give them bright orange jammies to wear, feed them at set times, dont allow them visitors unless it's visiting hours, take away their cigarettes (and drugs),. and in addition we periodically stab them with needles, poke tubes into various orifices and leave them at the mercy of the physiotherapists (affectionately known as the physioterrorists by some).
Indeed, the analogy seemed very fitting when I heard one of the nurses call out to another nurse (upon seeing three of the female patients in her bay sat out in chairs and not in bed) "Can you 'elp me get my free ladies back in bed?" In retrospect, perhaps this was merely her pronunciation and nothing to do with the analogy.
A few minutes later, a whooping arose from the corridor, and two nurses came flying by, riding the patient hoist! There then followed a crash and we peaked out to see both nurses on the floor next to the hoist, which had crashed into the wall at the end..
In other news, I have been honing my blood taking skills. Today one of the nurses asked me to take blood from a former IV drugs user. I'll admit it, my first thought was not about whether I would find a vein, but whether this chap might have Hep B, Hep C or HIV, and my next thought was whether he would think me rude if I wore two pairs of gloves to stick needles in him. I rationalised that actually, yes he is a high risk patient, but I have never had a needlestick injury and am not highly likely to stick myself this time either so didnt double glove. He seemed like a reasonable guy, very open about his past, and really glad to have left it all behind him (although says he still occasionally gets really painful abscesses at previous injection sites which is an unwelcome reminder). Of course, I couldnt find a vein anywhere so resorted to an arterial stab at the radial artery in the wrist. Halfway through the procedure he was very keen to tell me how he'd been tested for the above blood borne viruses and was clean.
One of the things I love about this job is the opportunity to meet interesting people I would never otherwise have contact with. It's a privilege to gain an insight into lives that have been so different from my own.
Indeed, the analogy seemed very fitting when I heard one of the nurses call out to another nurse (upon seeing three of the female patients in her bay sat out in chairs and not in bed) "Can you 'elp me get my free ladies back in bed?" In retrospect, perhaps this was merely her pronunciation and nothing to do with the analogy.
A few minutes later, a whooping arose from the corridor, and two nurses came flying by, riding the patient hoist! There then followed a crash and we peaked out to see both nurses on the floor next to the hoist, which had crashed into the wall at the end..
In other news, I have been honing my blood taking skills. Today one of the nurses asked me to take blood from a former IV drugs user. I'll admit it, my first thought was not about whether I would find a vein, but whether this chap might have Hep B, Hep C or HIV, and my next thought was whether he would think me rude if I wore two pairs of gloves to stick needles in him. I rationalised that actually, yes he is a high risk patient, but I have never had a needlestick injury and am not highly likely to stick myself this time either so didnt double glove. He seemed like a reasonable guy, very open about his past, and really glad to have left it all behind him (although says he still occasionally gets really painful abscesses at previous injection sites which is an unwelcome reminder). Of course, I couldnt find a vein anywhere so resorted to an arterial stab at the radial artery in the wrist. Halfway through the procedure he was very keen to tell me how he'd been tested for the above blood borne viruses and was clean.
One of the things I love about this job is the opportunity to meet interesting people I would never otherwise have contact with. It's a privilege to gain an insight into lives that have been so different from my own.
Tuesday, 20 September 2011
Dr Doctor, better warm it up first..
I happened upon a couple of nurses today, discussing the best approach to performing an enema on one of our most constipated patients. This was a repeat attempt, so the strategy was very important.
- You have to get the angle right [demonstrating possible angles with small bottle of enema solution]
- Yes yes, if you get the angle wrong then it just goes everywhere [voice of experience]
- Oh, and it's very important to warm it up first..
At this point the other nurse takes the bottle of enema solution and pops it down her uniform, lodging it somewhere in her ample bosom! I was somewhat aghast, but couldnt help laughing at the pair of them, so we all fell about, and next thing she tries to fish it out and the top flies off and she gets soaked in enema! Hilarious.
All these nursing tips one picks up on the wards..
- You have to get the angle right [demonstrating possible angles with small bottle of enema solution]
- Yes yes, if you get the angle wrong then it just goes everywhere [voice of experience]
- Oh, and it's very important to warm it up first..
At this point the other nurse takes the bottle of enema solution and pops it down her uniform, lodging it somewhere in her ample bosom! I was somewhat aghast, but couldnt help laughing at the pair of them, so we all fell about, and next thing she tries to fish it out and the top flies off and she gets soaked in enema! Hilarious.
All these nursing tips one picks up on the wards..
Saturday, 17 September 2011
Dr Doctor, the patient has fallen, and is unable to get up.
Just finished my second of three weekend late on-call shifts. This evening has been eventful. Firstly, weekends on call are generally a lot busier than weekdays on call because there are fewer staff on at the weekend so jobs get done later and there are usually more to hand over. So at the beginning of the shift I had a long list of things to do which required some prioritisation. A few of the jobs were things like checking blood levels of drugs such as digoxin and gentamicin, which have to be done at a certain time, others included a mountain of cannulas, a few bloods to take and check and a couple of drugs charts to be re-written.
I was busy attempting to take blood from one chap for a digoxin level, when I noticed the chap in the bed next to him stand up somewhat unsteadily. Now if patients are prone to falls, they often have a falls alarm attached to them and to the chair/bed so that if they try to stand up a siren gets activated and a nurse comes to tell them to sit back down. No such alarm sounded as this gent stood up so I carried on with my attempts to get blood. A split second later and the standing chap turns around and topples forward, landing on his face with a truly awful thud, and then the falls alarm sounds. Sirens wailing, I leapt to the gentleman's side, poor thing had sustained a rather large scalp laceration and was hosing blood all over the floor, flailing gently on his back and looking confused. Thankfully an army of nurses appeared and together we applied compression to the wound and hoisted him back into bed. I checked over the rest of him - no apparent C-spine tenderness, no bony tenderness over the hips or long bones. No blood coming from the ears. Checked his drug chart to see if he was on warfarin (he wasn't)
- warfarin + head injury = CT Scan. Instructed nurses to start regular neuro obs and bleeped my SHO for an opinion on whether to glue, steri-strip or suture the wound. We glued him back together and all was well. Went back and obtained somewhat delayed digoxin level.
Next job was to certify a death. On examination.. patient looks dead. Actually she kind of looked asleep, but very blue around the edges. I listened for heart sounds and breath sounds, felt for a central pulse, checked pupillary reflexes and response to supraorbital pressure, none of which were present (thank goodness otherwise this may have confused the issue). Told the patient/body to Rest in Peace as I was leaving and felt a little silly. Documented my examination in the notes plus time of death, the absence of a pacemaker and Rest in Peace. Felt a little sad.
Next job was to work out how to hide from nurses on the ward waiting to pounce with additional jobs for me to do, while continuing to carry out the jobs on the ward I already needed to do. Failed, and picked up a review of a patient with high blood sugars (around 27, normal being roughly 3-7). Reason for admission of this patient was.. high blood sugars. Chances of me, the inexperienced FY1, managing to single handedly regulate this patient's blood sugars over the course of one on call shift were slim. Also, I find prescribing insulin a little scary. It's a dangerous drug and can certainly kill people in overdose. There are many many different preparations, all with different durations of action, and I really wasn't quite sure what to do. Cue time spent with the BNF (drug book) and a phone call to my SHO for advice. We settled on a small stat dose of 4 units of Actrapid (short acting insulin) alongside her regular intermediate acting insulin.
Managed to escape the Elderly Care nurses to take blood from an outlying patient near the end of the shift. As most NHS hospitals tend to be on "black alert" due to a shortage of beds, some of the less sick patients from one department can end up seemingly in any other part of the hospital. This chap for example, was parked in Urology. I found another chap in Obs and Gynae on yesterday's shift! I'm not sure what happens after black alert.. must be brown alert!
I was busy attempting to take blood from one chap for a digoxin level, when I noticed the chap in the bed next to him stand up somewhat unsteadily. Now if patients are prone to falls, they often have a falls alarm attached to them and to the chair/bed so that if they try to stand up a siren gets activated and a nurse comes to tell them to sit back down. No such alarm sounded as this gent stood up so I carried on with my attempts to get blood. A split second later and the standing chap turns around and topples forward, landing on his face with a truly awful thud, and then the falls alarm sounds. Sirens wailing, I leapt to the gentleman's side, poor thing had sustained a rather large scalp laceration and was hosing blood all over the floor, flailing gently on his back and looking confused. Thankfully an army of nurses appeared and together we applied compression to the wound and hoisted him back into bed. I checked over the rest of him - no apparent C-spine tenderness, no bony tenderness over the hips or long bones. No blood coming from the ears. Checked his drug chart to see if he was on warfarin (he wasn't)
- warfarin + head injury = CT Scan. Instructed nurses to start regular neuro obs and bleeped my SHO for an opinion on whether to glue, steri-strip or suture the wound. We glued him back together and all was well. Went back and obtained somewhat delayed digoxin level.
Next job was to certify a death. On examination.. patient looks dead. Actually she kind of looked asleep, but very blue around the edges. I listened for heart sounds and breath sounds, felt for a central pulse, checked pupillary reflexes and response to supraorbital pressure, none of which were present (thank goodness otherwise this may have confused the issue). Told the patient/body to Rest in Peace as I was leaving and felt a little silly. Documented my examination in the notes plus time of death, the absence of a pacemaker and Rest in Peace. Felt a little sad.
Next job was to work out how to hide from nurses on the ward waiting to pounce with additional jobs for me to do, while continuing to carry out the jobs on the ward I already needed to do. Failed, and picked up a review of a patient with high blood sugars (around 27, normal being roughly 3-7). Reason for admission of this patient was.. high blood sugars. Chances of me, the inexperienced FY1, managing to single handedly regulate this patient's blood sugars over the course of one on call shift were slim. Also, I find prescribing insulin a little scary. It's a dangerous drug and can certainly kill people in overdose. There are many many different preparations, all with different durations of action, and I really wasn't quite sure what to do. Cue time spent with the BNF (drug book) and a phone call to my SHO for advice. We settled on a small stat dose of 4 units of Actrapid (short acting insulin) alongside her regular intermediate acting insulin.
Managed to escape the Elderly Care nurses to take blood from an outlying patient near the end of the shift. As most NHS hospitals tend to be on "black alert" due to a shortage of beds, some of the less sick patients from one department can end up seemingly in any other part of the hospital. This chap for example, was parked in Urology. I found another chap in Obs and Gynae on yesterday's shift! I'm not sure what happens after black alert.. must be brown alert!
Tuesday, 13 September 2011
Dr Doctor, maggots in the fridge!
Witnessed an amusing exchange between two of our nurses this lunchtime. One is tall, somewhat rotund female and black, the other is short, seasoned, male and Sri Lankan.
Large black nurse comes out of the kitchen behind the nurses station with much gesticulation at diminutive, elderly Sri Lankan Nurse:
- WHY YOU PUT DEM MAGGOTS IN DA FRIIIIGE HUH?
- dee maggots needs to be keeping cold
- MY LONCH is in da friidge youknowwhaamsayin??
- please, I put dee maggots nowhere near your lunch!
- Oh. Nu-uh. You put dem on da shelf ABOVV my lonch.
- maybe thees is true, but its no problem.
- Oh, I tink it be a problemm - they was in a TESCOBAG
- please, what is dee problem with a Tesco bag?
- My LONCH was in a Tescobag. I open da Tescobag and I tink Oh. Da maggots has eaten my LONCH!
Turns out we have a patient with a particularly nasty sacral bedsore. The NHS, perhaps as part of cost-cutting manoeuvres, has begun to resort to medieval management of such ailments and as such 'maggot therapy' is becoming more widely used within our hospitals. As they only eat necrotic tissue, they are in fact extremely effective at removing rotten flesh without damaging healthy tissue, thus allowing wounds to heal cleanly. Apparently, they need to be kept cool before use.
Large black nurse comes out of the kitchen behind the nurses station with much gesticulation at diminutive, elderly Sri Lankan Nurse:
- WHY YOU PUT DEM MAGGOTS IN DA FRIIIIGE HUH?
- dee maggots needs to be keeping cold
- MY LONCH is in da friidge youknowwhaamsayin??
- please, I put dee maggots nowhere near your lunch!
- Oh. Nu-uh. You put dem on da shelf ABOVV my lonch.
- maybe thees is true, but its no problem.
- Oh, I tink it be a problemm - they was in a TESCOBAG
- please, what is dee problem with a Tesco bag?
- My LONCH was in a Tescobag. I open da Tescobag and I tink Oh. Da maggots has eaten my LONCH!
Turns out we have a patient with a particularly nasty sacral bedsore. The NHS, perhaps as part of cost-cutting manoeuvres, has begun to resort to medieval management of such ailments and as such 'maggot therapy' is becoming more widely used within our hospitals. As they only eat necrotic tissue, they are in fact extremely effective at removing rotten flesh without damaging healthy tissue, thus allowing wounds to heal cleanly. Apparently, they need to be kept cool before use.
Friday, 9 September 2011
Dr Doctor by the way, the patient looks moribund..
Last evening on call and I get completely swamped with jobs from the very start. All the small jobs like reviewing bloods, taking outstanding bloods and checking chest x-rays etc get handed over to the F1 and not to the SHOs because people dont want to bother the SHOs with them. Add to this three new stroke patients to clerk, one catheter to replace, one patient that had fallen out of bed and an abundance of warfarin doses to review the INR and change accordingly, and I was running around like a mad thing, hiding under the desks of the nurses stations on each ward to avoid nurses with yet more fluid charts to fill out.
In the midst of the never ending bleeps came a call from one of the matrons.
- Hello doctor, just checked this lady's bloods and her sodium is 166 [very high].
- Have you got her current obs?
- No, but she looks moribund.
- Er.. I'll come and see her, please start a set of obs and I'll be there.
I figured that matrons by definition have a wealth of experience behind them, and despite the slightly pants referral, if matron says patient looks near death the patient may well need looking at. When I arrived a suitably helpful nurse was halfway through taking the obs and the patient looked sick. Perhaps not moribund, but sick and lying slumped down in bed. She was relatively unresponsive with a GCS around 7 [eek, this could become an airway problem] her pulse was 100, BP 115/80, cap refill 4 secs, apyrexial, RR 30 sats 84% on 2L oxygen [EEK, instructed nurse to please immediately fetch another venturi mask to up her oxygen to 35%] and her chest sounded full of fluid.
So I got her sat up in bed to make it easier for her to breathe, left her on the oxygen (sats were improving to around 94% by now and her GCS came up to around 11 with her being a bit less hypoxic) and rang my SHO who came to see her. Rechecked her bloods, sodium was indeed 166 up from 155 a couple of days before, and on reviewing her fluids chart noticed she hadnt been given any of the fluids she'd been prescribed for the past four days!? Probably why her sodium was so high - she was very dry. Prescribed some Haartman's solution to run in over 10 hours, could have gone for dextrose but after discussing with the seniors we didnt want to correct the sodium level by rehydrating too quickly because this can cause cerebral oedema. Once she was stable the SHO insisted we go for a cup of tea in the doctors mess and divide up the jobs I had left, thank goodness!
I heard the night team diagnosed simultaneous pulmonary oedema (waterlogged lungs) and intravascular depletion (empty circulation) which led them to treat her paradoxically with frusemide (a diuretic that makes wee out more fluid but is also acts in other ways to reduce pulmonary oedema) and fluids to try to get the fluid off her lungs and into her circulation.
In the midst of the never ending bleeps came a call from one of the matrons.
- Hello doctor, just checked this lady's bloods and her sodium is 166 [very high].
- Have you got her current obs?
- No, but she looks moribund.
- Er.. I'll come and see her, please start a set of obs and I'll be there.
I figured that matrons by definition have a wealth of experience behind them, and despite the slightly pants referral, if matron says patient looks near death the patient may well need looking at. When I arrived a suitably helpful nurse was halfway through taking the obs and the patient looked sick. Perhaps not moribund, but sick and lying slumped down in bed. She was relatively unresponsive with a GCS around 7 [eek, this could become an airway problem] her pulse was 100, BP 115/80, cap refill 4 secs, apyrexial, RR 30 sats 84% on 2L oxygen [EEK, instructed nurse to please immediately fetch another venturi mask to up her oxygen to 35%] and her chest sounded full of fluid.
So I got her sat up in bed to make it easier for her to breathe, left her on the oxygen (sats were improving to around 94% by now and her GCS came up to around 11 with her being a bit less hypoxic) and rang my SHO who came to see her. Rechecked her bloods, sodium was indeed 166 up from 155 a couple of days before, and on reviewing her fluids chart noticed she hadnt been given any of the fluids she'd been prescribed for the past four days!? Probably why her sodium was so high - she was very dry. Prescribed some Haartman's solution to run in over 10 hours, could have gone for dextrose but after discussing with the seniors we didnt want to correct the sodium level by rehydrating too quickly because this can cause cerebral oedema. Once she was stable the SHO insisted we go for a cup of tea in the doctors mess and divide up the jobs I had left, thank goodness!
I heard the night team diagnosed simultaneous pulmonary oedema (waterlogged lungs) and intravascular depletion (empty circulation) which led them to treat her paradoxically with frusemide (a diuretic that makes wee out more fluid but is also acts in other ways to reduce pulmonary oedema) and fluids to try to get the fluid off her lungs and into her circulation.
Wednesday, 7 September 2011
Dr Doctor get it yourself!
Now call me naive, but I genuinely thought that nurses are generally helpful beings, willing to assist doctors in caring for sick patients. There was a mixed bag of nurses on duty yesterday evening. I was very much swamped with tasks, from clerking in new patients to reviewing bloods to taking bloods to reviewing medications. I was very much impressed by one nurse who was willing to take a set of bloods for me, from a difficult to bleed patient that she was used to bleeding. She saved me a good 10-15 minutes for which I was extremely grateful. So my faith in nurses was high around the middle of my shift.
When I finally had a minute to inhale some of my "packed dinner" I was sat in the doctors mess when my bleep went off again. Now I had heard rumours that occasionally handovers are very badly done, but had yet to experience it until this moment. The conversation went along these lines:
- Hello, it's the F1 on call.
- Hello this is one of the nurses calling from the ward, I've got a patient with a temperature of 38.5.
[Dead silence, as I wait to hear the rest of the obs and the reason for the call]
- What are the rest of the obs?
- Um, I dont know, we're just doing them.
- Alright, why is this patient in hospital?
- Um, I'm not looking after them so I dont know.
[Silence, while I wait for her to look through the notes]
- Er.. she has a UTI
- What were her last set of obs like?
- I'll just check. I'm not sure where they've been written down.. I think she had a temperature earlier too.
- So you've called about the spiking temperature, is there anything else that's concerning you about this patient?
- Well, yes, the temperature.
- Ok, I need to know if this patient is unwell enough for me to need to come and see her, so maybe you could ring me back when you've done the current obs.
- Alright, I'll do that.
I looked at the phone in puzzled disbelief, still not sure why I had been called. I wasnt particularly concerned, and was expecting her obs to be normalish and that I probably wouldnt need to review her. Five minutes later the nurse calls me back.
- Her temperature is 38.5. Her blood pressure is 147/85. Her heart rate is 98.
[my ears started to prick up at this point]
Her sats are 94%. Her respiratory rate is 33.
[my ears sprang to attention and I sat up rather straighter]
- Is she on any oxygen?
- No
- Please put her on 28 % oxygen and I'll come and see her now.
It took me a good five minutes to traverse the hospital to the ward, and when I arrived there was an abundance of nurses at the nurses station, all of whom ignored me.
- Hello, I'm the on call F1, who was I speaking to?
- Oh that was me [this nurse looked seasoned enough that she ought to know how to give a proper handover] I havent got around to putting the oxygen on yet! [And she laughed.]
- Right. Where is this patient?
I had been mentally running through my approach to the sick patient on my way there.
1 Do they look sick?
2 Assess airway breathing and circulation and treat stuff as I find it.
3 Further investigations
4 Differential diagnosis and plan
So this patient looked sick, she was obviously breathing fast and was quite drowsy. The nurse hovered next to me, not looking like she was in any rush to apply the oxygen. So I asked her again. I was at this point feeling somewhat frustrated, and concerned both about the patient and the lack of understanding of the clinical situation that the nurses here seemed to have. It was the right thing to do to call me, but they'd done so for the wrong reason and were completely unprepared to give me the information I really needed.
I assessed the patient, decided she wasnt shocked but might have a chest infection, ordered a chest x-ray, took blood cultures and decided to do an arterial blood gas sample. I asked a different nurse to please find me a blood gas syringe and she was singularly unhelpful, and flatly refused to go to the next ward over to find one, in fact saying "you'll have to get it yourself'. Here was me thinking that actually, there are about 6 nurses standing around the nurses station doing nothing, and me running around trying to sort out a sick patient, and maybe if I need a piece of equipment it might be logical, helpful, and safer for the patient if one of them were to go and do it. I weighed up the time I would waste arguing with her versus the stability of patient and went myself. I was not impressed, and was disappointed that my idealistic view of us all working as a team for the good of the patients had been slightly tarnished. Had the patient been much sicker I would have insisted that she go, but it's not (yet?) in my nature to pull rank.
Having done as much as I could I rang my SHO for a more senior review. By the time my SHO arrived, the patient's respiratory rate had decreased to 28 and her sats had improved, so I'd at least fixed her a little bit with the (eventual application of) oxygen.
When I finally had a minute to inhale some of my "packed dinner" I was sat in the doctors mess when my bleep went off again. Now I had heard rumours that occasionally handovers are very badly done, but had yet to experience it until this moment. The conversation went along these lines:
- Hello, it's the F1 on call.
- Hello this is one of the nurses calling from the ward, I've got a patient with a temperature of 38.5.
[Dead silence, as I wait to hear the rest of the obs and the reason for the call]
- What are the rest of the obs?
- Um, I dont know, we're just doing them.
- Alright, why is this patient in hospital?
- Um, I'm not looking after them so I dont know.
[Silence, while I wait for her to look through the notes]
- Er.. she has a UTI
- What were her last set of obs like?
- I'll just check. I'm not sure where they've been written down.. I think she had a temperature earlier too.
- So you've called about the spiking temperature, is there anything else that's concerning you about this patient?
- Well, yes, the temperature.
- Ok, I need to know if this patient is unwell enough for me to need to come and see her, so maybe you could ring me back when you've done the current obs.
- Alright, I'll do that.
I looked at the phone in puzzled disbelief, still not sure why I had been called. I wasnt particularly concerned, and was expecting her obs to be normalish and that I probably wouldnt need to review her. Five minutes later the nurse calls me back.
- Her temperature is 38.5. Her blood pressure is 147/85. Her heart rate is 98.
[my ears started to prick up at this point]
Her sats are 94%. Her respiratory rate is 33.
[my ears sprang to attention and I sat up rather straighter]
- Is she on any oxygen?
- No
- Please put her on 28 % oxygen and I'll come and see her now.
It took me a good five minutes to traverse the hospital to the ward, and when I arrived there was an abundance of nurses at the nurses station, all of whom ignored me.
- Hello, I'm the on call F1, who was I speaking to?
- Oh that was me [this nurse looked seasoned enough that she ought to know how to give a proper handover] I havent got around to putting the oxygen on yet! [And she laughed.]
- Right. Where is this patient?
I had been mentally running through my approach to the sick patient on my way there.
1 Do they look sick?
2 Assess airway breathing and circulation and treat stuff as I find it.
3 Further investigations
4 Differential diagnosis and plan
So this patient looked sick, she was obviously breathing fast and was quite drowsy. The nurse hovered next to me, not looking like she was in any rush to apply the oxygen. So I asked her again. I was at this point feeling somewhat frustrated, and concerned both about the patient and the lack of understanding of the clinical situation that the nurses here seemed to have. It was the right thing to do to call me, but they'd done so for the wrong reason and were completely unprepared to give me the information I really needed.
I assessed the patient, decided she wasnt shocked but might have a chest infection, ordered a chest x-ray, took blood cultures and decided to do an arterial blood gas sample. I asked a different nurse to please find me a blood gas syringe and she was singularly unhelpful, and flatly refused to go to the next ward over to find one, in fact saying "you'll have to get it yourself'. Here was me thinking that actually, there are about 6 nurses standing around the nurses station doing nothing, and me running around trying to sort out a sick patient, and maybe if I need a piece of equipment it might be logical, helpful, and safer for the patient if one of them were to go and do it. I weighed up the time I would waste arguing with her versus the stability of patient and went myself. I was not impressed, and was disappointed that my idealistic view of us all working as a team for the good of the patients had been slightly tarnished. Had the patient been much sicker I would have insisted that she go, but it's not (yet?) in my nature to pull rank.
Having done as much as I could I rang my SHO for a more senior review. By the time my SHO arrived, the patient's respiratory rate had decreased to 28 and her sats had improved, so I'd at least fixed her a little bit with the (eventual application of) oxygen.
Tuesday, 6 September 2011
Dr Doctor you're on call.
So it's back to the wards, and I've been thrown back in on the late shift on call. This entails starting at 1430 with my usual ward team, then attending a 1630 handover from the elderly care wards and the medical wards about sick patients and jobs that the day team havent managed to do, picking up the on call bleep and waiting for it to go off. After 1800 the day team have mostly gone so the elderly care wards are looked after by the F1 (me) and two SHOs.
First job, believe it or not, was to do a PR examination on one of the new patients who had a falling haemoglobin level to check that he didnt have any malaena (altered blood in the stools) that might indicate GI bleeding before giving him high dose aspirin. Now my experience of PR examination from medical school is limited to one hour in the clinical skills lab with a plastic model arse, the rubberised arse section of which got stuck on my finger and came off when I tried to withdraw, resulting in the prostate falling out and bouncing around the room. My only previous attempt on a patient ended rather messily with a proctoscope being farted vigorously back out at me (the patient was quite unharmed I can assure you). So of course I didnt quite relish the idea of performing this procedure on the dear little old man in front of me. Despite having never met him before I had to gain his trust, gain his consent, put him at ease and perform the procedure competently and professionally.
My tips - make sure the patient is fully informed about the procedure and why it needs to be done (not only does this build rapport but is a legal necessity), take a nurse to chaperone, talk through what you're doing, be quick but thorough, and for heaven's sake double glove (take the first glove off when you withdraw so that you can clean the patient with a clean gloved hand). Document everything in the notes afterwards, especially that you gained consent, who the chaperone was, and your examination findings.
Other jobs included reviewing an outlying patient on warfarin with an INR of 5.0 (this means she's over-anticoagulated and the warfarin dose needs changing). I went to see her, asked if she had noticed any bleeding from anywhere, examined her and changed the dose according to Trust Guidelines.
I also had to review a couple of x-rays and a heap of bloods (normally this is done by the day team but thanks to the phlebotomists not bleeding the patients on some of the wards till 1600 none of the results were back. I found only one interesting result - a sodium level that had dropped overnight from 133 (normalish) to 126. The patient was well and not confused, and none of the medications she'd been started on recently could have caused the drop so I wrote the results in her notes with a plan to repeat the sodium next day.
Handed over to the night team at 2200, fairly uneventful shift.
First job, believe it or not, was to do a PR examination on one of the new patients who had a falling haemoglobin level to check that he didnt have any malaena (altered blood in the stools) that might indicate GI bleeding before giving him high dose aspirin. Now my experience of PR examination from medical school is limited to one hour in the clinical skills lab with a plastic model arse, the rubberised arse section of which got stuck on my finger and came off when I tried to withdraw, resulting in the prostate falling out and bouncing around the room. My only previous attempt on a patient ended rather messily with a proctoscope being farted vigorously back out at me (the patient was quite unharmed I can assure you). So of course I didnt quite relish the idea of performing this procedure on the dear little old man in front of me. Despite having never met him before I had to gain his trust, gain his consent, put him at ease and perform the procedure competently and professionally.
My tips - make sure the patient is fully informed about the procedure and why it needs to be done (not only does this build rapport but is a legal necessity), take a nurse to chaperone, talk through what you're doing, be quick but thorough, and for heaven's sake double glove (take the first glove off when you withdraw so that you can clean the patient with a clean gloved hand). Document everything in the notes afterwards, especially that you gained consent, who the chaperone was, and your examination findings.
Other jobs included reviewing an outlying patient on warfarin with an INR of 5.0 (this means she's over-anticoagulated and the warfarin dose needs changing). I went to see her, asked if she had noticed any bleeding from anywhere, examined her and changed the dose according to Trust Guidelines.
I also had to review a couple of x-rays and a heap of bloods (normally this is done by the day team but thanks to the phlebotomists not bleeding the patients on some of the wards till 1600 none of the results were back. I found only one interesting result - a sodium level that had dropped overnight from 133 (normalish) to 126. The patient was well and not confused, and none of the medications she'd been started on recently could have caused the drop so I wrote the results in her notes with a plan to repeat the sodium next day.
Handed over to the night team at 2200, fairly uneventful shift.
Monday, 5 September 2011
Dr Doctor there's nothing more we can do.
My last day in ITU was somewhat sad. We had a lady who was day 2 post out of hospital cardiac arrest who we had been cooling (it has been shown that cooling people after cardiac arrest can improve neurological outcomes) and then rewarmed her overnight. In the morning when I arrived she began fitting, which is never a good sign. The decision was made after discussion with the family that she should be kept comfortable and we would let her pass away.
That afternoon I was sat writing in some notes at the nurses station when out of nowhere the monitor that shows all of the patient's heart traces started going completely bananas, flashing red and black and making siren noises and screaming VT! VT! because the patient had gone into one of the cardiac arrest rhythms. It gave me such a fright that I literally leapt out my seat, surprised that I myself had not been sent into a cardiac arrest rhythm.
The consultant sat next me very calmly (ITU and anaesthetic consultants are always calm, without exception, something to do with the vast quantity of experience of very sick patients and superhuman level of knowledge they accumulate) wafted me back down into my seat. "We wont be treating this," he said, "this was expected."
Over the next ten minutes I found it both interesting and extremely sad to watch the wavy lines of this lady's heart trace deteriorate from VT into VF, occasionally back into sinus rhythm and then get gradually slower and slower until the last blip vanished and she was in asystole. It's quite unusual to watch this because in most patients people would be actively resuscitating and those not for resuscitation are not usually monitored.
That afternoon I was sat writing in some notes at the nurses station when out of nowhere the monitor that shows all of the patient's heart traces started going completely bananas, flashing red and black and making siren noises and screaming VT! VT! because the patient had gone into one of the cardiac arrest rhythms. It gave me such a fright that I literally leapt out my seat, surprised that I myself had not been sent into a cardiac arrest rhythm.
The consultant sat next me very calmly (ITU and anaesthetic consultants are always calm, without exception, something to do with the vast quantity of experience of very sick patients and superhuman level of knowledge they accumulate) wafted me back down into my seat. "We wont be treating this," he said, "this was expected."
Over the next ten minutes I found it both interesting and extremely sad to watch the wavy lines of this lady's heart trace deteriorate from VT into VF, occasionally back into sinus rhythm and then get gradually slower and slower until the last blip vanished and she was in asystole. It's quite unusual to watch this because in most patients people would be actively resuscitating and those not for resuscitation are not usually monitored.
Tuesday, 30 August 2011
Dr Doctor please fill in the death certificate.
So today I had the responsibility of filling in my first death certificate and cremation form. The patient was a 75 year old lady who had come into the Emergency Department with sudden onset severe headache and collapse and was found to have had a massive unsurvivable intracranial haemorrhage. She came to ITU for some TLC and palliation in the absence of anywhere else for her to go and passed away peacefully a couple of days later.
Filling in the cremation form is a fairly long process as it has to be very detailed because once the body has been cremated there's no reassembling it to perform any further post mortem tests. The doctor also gets paid around £80 for taking the time to fill it in - "Ash Cash".
Part of the process is to examine the body (which I wasnt quite expecting) so I took a rather apprehensive medical student to the morgue for moral support and was met by an utterly stereotypical morgue assistant with somewhat squinty eyes and an unusual gait. He led us into an enormous fridge lined room and located my lady who, typically, had been placed in the top slot of a four body high fridge. "You'll be wanting some steps," he growled. I looked up to the top slot and had visions of me having to clamber on top of the occupants of the other shelves to examine my lady. "Yes please".
The steps turned out to be ancient and rickety so I spent the duration of my examination wobbling and earnestly trying not to fall on top of the body. The patient looked as if she were asleep with her eyes open, and felt extremely cold and rubbery when I was feeling for a pacemaker. Having performed a "full external examination", I thanked Lurch and we left, to go and fill in the rest of the paperwork.
Filling in the cremation form is a fairly long process as it has to be very detailed because once the body has been cremated there's no reassembling it to perform any further post mortem tests. The doctor also gets paid around £80 for taking the time to fill it in - "Ash Cash".
Part of the process is to examine the body (which I wasnt quite expecting) so I took a rather apprehensive medical student to the morgue for moral support and was met by an utterly stereotypical morgue assistant with somewhat squinty eyes and an unusual gait. He led us into an enormous fridge lined room and located my lady who, typically, had been placed in the top slot of a four body high fridge. "You'll be wanting some steps," he growled. I looked up to the top slot and had visions of me having to clamber on top of the occupants of the other shelves to examine my lady. "Yes please".
The steps turned out to be ancient and rickety so I spent the duration of my examination wobbling and earnestly trying not to fall on top of the body. The patient looked as if she were asleep with her eyes open, and felt extremely cold and rubbery when I was feeling for a pacemaker. Having performed a "full external examination", I thanked Lurch and we left, to go and fill in the rest of the paperwork.
Thursday, 25 August 2011
Dr Doctor my EMG is farting!
We have a very interesting patient on ITU at the moment, who presented with severe rhabdomyolysis (muscle damage) leading to leakage of myoglobin (muscle protein) which caused severe renal failure (because it damages the kidneys). He is interesting because nobody can work out quite why this has happened to him.
One of the exceptionally intelligent consultant electrophysiologists came to review him and test the nerve conduction in his muscles. This involved attaching electrodes to the skin and stimulating the muscles and turning the response into a wavy line pattern on a screen and into a sound signal. He happened to be doing the test during our ward round so we all gathered around to watch.
He checked the monitor, turned the volume up and sent a signal to stimulate the muscle, and there erupted from the machine at about 60 decibels what can only be described as an enormous, prolonged bout of flatulence that echoed around the otherwise relatively quiet ITU! It almost awoke most of the sedated patients, and agitated the poor chap in the next bay to such an extent that he extubated himself! Poor thing looked ever so confused.
Matters were not helped by me being the only one who seemingly could not control my giggles, and the registrar who offered a finger with the old adage "pull my finger" as the seasoned consultant repeatedly stimulated the poor patient's muscle with the same effect, earnestly explaining how this noise meant the patient may well have myotonic dystrophy.
Copy and paste the link below to hear something similar.
http://www.youtube.com/watch?v=xMAu6sZ7ROs
One of the exceptionally intelligent consultant electrophysiologists came to review him and test the nerve conduction in his muscles. This involved attaching electrodes to the skin and stimulating the muscles and turning the response into a wavy line pattern on a screen and into a sound signal. He happened to be doing the test during our ward round so we all gathered around to watch.
He checked the monitor, turned the volume up and sent a signal to stimulate the muscle, and there erupted from the machine at about 60 decibels what can only be described as an enormous, prolonged bout of flatulence that echoed around the otherwise relatively quiet ITU! It almost awoke most of the sedated patients, and agitated the poor chap in the next bay to such an extent that he extubated himself! Poor thing looked ever so confused.
Matters were not helped by me being the only one who seemingly could not control my giggles, and the registrar who offered a finger with the old adage "pull my finger" as the seasoned consultant repeatedly stimulated the poor patient's muscle with the same effect, earnestly explaining how this noise meant the patient may well have myotonic dystrophy.
Copy and paste the link below to hear something similar.
http://www.youtube.com/watch?v=xMAu6sZ7ROs
Tuesday, 16 August 2011
Dr Doctor please refer this patient..
Patients generally land in ITU with a complicated medical history and numerous ongoing problems, some of which may have been investigated in a completely different hospital. The challenge is often to obtain the relevant scan report/microbiology result/clinical opinion from said hospital, in as few moves as possible. This involves a LOT of time on the phone, and much use of the ladies on switchboard.
Yesterday I was tasked with obtaining scan reports and haematology results from my patient's first hospital and then referring them to the haematologists in our hospital. This involved a lot of talking to switchboard. Now on the whole switchboard ladies are fabulous, but yesterday I kept getting through to World's Grumpiest Operator. When I asked to be put through to Hospital X, instead of pushing the one button that would have transferred me simply and easily she instead gave me the direct dial number in a disparaging tone and slammed the phone down. Obediently I used the direct dial number each time I needed to get through to Hospital X the numerous times it took me to get the information I needed (or rather discover the haematology results arent back yet and the scan report is still unverified). Then it was with trepidation that I had to phone our Switchboard to get the bleep number of the on-call haematology registrar which World's Grumpiest Operator snapped down the phone at me in such a way that I almost apologised for not having already known the number myself.
So I bleeped the number and who should phone back but a similarly grumpy grumpy chap who introduced himself as the mumblemumble registrar. Considering that I had managed to get hold of some sort of registrar and on balance they were probably from haematology I proceeded to present the case, emphasising our concerns over the patient's low platelet count and low white cell count and low haemoglobin and finished by saying we would really appreciate it if he could come and review the patient. There was a long pause and then a somewhat exasperated "You do know you're talking to a UROLOGIST right?" How embarrassing - completely wrong person, and a surgeon at that - they're far too busy to listen to pointless referrals! Cue much flustered apologising.
Who knows, maybe he'd also pissed off World's Grumpiest Operator and she decided to get a rise out of both of us!
Yesterday I was tasked with obtaining scan reports and haematology results from my patient's first hospital and then referring them to the haematologists in our hospital. This involved a lot of talking to switchboard. Now on the whole switchboard ladies are fabulous, but yesterday I kept getting through to World's Grumpiest Operator. When I asked to be put through to Hospital X, instead of pushing the one button that would have transferred me simply and easily she instead gave me the direct dial number in a disparaging tone and slammed the phone down. Obediently I used the direct dial number each time I needed to get through to Hospital X the numerous times it took me to get the information I needed (or rather discover the haematology results arent back yet and the scan report is still unverified). Then it was with trepidation that I had to phone our Switchboard to get the bleep number of the on-call haematology registrar which World's Grumpiest Operator snapped down the phone at me in such a way that I almost apologised for not having already known the number myself.
So I bleeped the number and who should phone back but a similarly grumpy grumpy chap who introduced himself as the mumblemumble registrar. Considering that I had managed to get hold of some sort of registrar and on balance they were probably from haematology I proceeded to present the case, emphasising our concerns over the patient's low platelet count and low white cell count and low haemoglobin and finished by saying we would really appreciate it if he could come and review the patient. There was a long pause and then a somewhat exasperated "You do know you're talking to a UROLOGIST right?" How embarrassing - completely wrong person, and a surgeon at that - they're far too busy to listen to pointless referrals! Cue much flustered apologising.
Who knows, maybe he'd also pissed off World's Grumpiest Operator and she decided to get a rise out of both of us!
Friday, 12 August 2011
Dr Doctor I've drunk antifreeze!
The ITU team often gets called to the Emergency Department to assess patients who may or may not need not be managed in ITU. Today's offering was a 45 year old gentleman who had imbibed nearly a litre of antifreeze the previous day and decided to keep quiet about it. He eventually started feeling unwell and told an ex-partner (there's always an ex-partner) who phoned his parents who brought him to hospital.
When we saw him he had fairly deranged blood gases (was moderately acidaemic with a low PCO2) and was hyperventilating to compensate. So from a physiological point of view, quite an interesting case. Helpfully he had washed it all down with a bottle of red wine, and, ironically, alcohol (ethanol) being the antidote to antifreeze had slowed down the process of poisoning himself.
It's interesting the effect self harm cases has on the medical team. Truly suicidal people tend just to get on with it and are sadly found deceased or beyond help. Similarly truly depressed people tend not to tell anyone about how bad they're feeling. The Emergency Department has to deal with a huge number of people "crying for help" on a daily basis, taking ineffectual overdoses or cutting themselves and presenting immediately for TLC. The medical team's duty of care means a lot of time and resources are spent patching these patients up and either referring them to mental health services or discharging them home where they become down and desperate and repeat the cycle of turning up at hospital where people will listen to and care for them. It can be hugely frustrating trying to help somebody who doesnt want to be helped or who are perceived as "attention seeking".
Mr Ethylene Glycol was quite difficult to manage, partly due to his co-existing needle phobia not going well with the requirement to obtain several blood samples for ethylene glycol/methanol levels (in fact the lab rejected the samples saying they "dont do ethylene glycol or methanol levels"), partly because by this point he was realising the seriousness of what he had done and was feeling very unwell. While it is understandable that the chap was frightened and most of his acting up was probably due to this, it is also very difficult to continue to empathise when you know you have to get that needle/line/catheter into him in order to administer the correct treatment.
Speaking of treatment, there's a new antidote to ethylene glycol called fomepizole which costs £4000 per vial. Apparently it works better than ethanol (by irreversibly inhibiting the relevant enzymes) and is thus the best treatment for the patient, but with the NHS needing to save money perhaps there would have been justification for simply filling the chap with vodka! Indeed most Emergency Departments have a bottle of some spirit somewhere for the antifreeze/methanol drinkers out there, and not for the stressed out doctors.
When we saw him he had fairly deranged blood gases (was moderately acidaemic with a low PCO2) and was hyperventilating to compensate. So from a physiological point of view, quite an interesting case. Helpfully he had washed it all down with a bottle of red wine, and, ironically, alcohol (ethanol) being the antidote to antifreeze had slowed down the process of poisoning himself.
It's interesting the effect self harm cases has on the medical team. Truly suicidal people tend just to get on with it and are sadly found deceased or beyond help. Similarly truly depressed people tend not to tell anyone about how bad they're feeling. The Emergency Department has to deal with a huge number of people "crying for help" on a daily basis, taking ineffectual overdoses or cutting themselves and presenting immediately for TLC. The medical team's duty of care means a lot of time and resources are spent patching these patients up and either referring them to mental health services or discharging them home where they become down and desperate and repeat the cycle of turning up at hospital where people will listen to and care for them. It can be hugely frustrating trying to help somebody who doesnt want to be helped or who are perceived as "attention seeking".
Mr Ethylene Glycol was quite difficult to manage, partly due to his co-existing needle phobia not going well with the requirement to obtain several blood samples for ethylene glycol/methanol levels (in fact the lab rejected the samples saying they "dont do ethylene glycol or methanol levels"), partly because by this point he was realising the seriousness of what he had done and was feeling very unwell. While it is understandable that the chap was frightened and most of his acting up was probably due to this, it is also very difficult to continue to empathise when you know you have to get that needle/line/catheter into him in order to administer the correct treatment.
Speaking of treatment, there's a new antidote to ethylene glycol called fomepizole which costs £4000 per vial. Apparently it works better than ethanol (by irreversibly inhibiting the relevant enzymes) and is thus the best treatment for the patient, but with the NHS needing to save money perhaps there would have been justification for simply filling the chap with vodka! Indeed most Emergency Departments have a bottle of some spirit somewhere for the antifreeze/methanol drinkers out there, and not for the stressed out doctors.
Wednesday, 10 August 2011
Dr Doctor there's rice in the ET Tube!
Have somehow landed myself four weeks in ITU. Being essentially supernumerary I get to jog around the hospital with the SHOs whenever the cardiac arrest bleeps go off. Often, we arrive on scene and the patient is actually fine, either because the fantastic medical team have got there before us and fixed the patient, or (more often than not) a patient has prostrated themselves in the main entrance and receptionist has interpreted a faint or a reluctance to move as a cardiac arrest.
Had 3 arrest bleeps in the space of about an hour yesterday, one was a post lunch vasovagal episode in an elderly chap (medical registrar's advice was "administer less lunch"), one was a patient with renal colic on the floor in main reception (needed some analgesia and a porter to urology) and the last one was a chap who'd managed to simultaneously choke on lunch, vomit everywhere, aspirate and start fitting. Cue real ITU action involving securing the airway by RSI and intubation, which was made much more difficult by the resurgence of lunch from the lungs. Much suctioning later and he was ready for an arterial line placement and transfer to CT for a brain scan. The chap was ventilated on ITU overnight and extubated this afternoon and not looking too bad. His lunch continues to resurface periodically.
Conclusion - hospital lunches are dangerous.
Had 3 arrest bleeps in the space of about an hour yesterday, one was a post lunch vasovagal episode in an elderly chap (medical registrar's advice was "administer less lunch"), one was a patient with renal colic on the floor in main reception (needed some analgesia and a porter to urology) and the last one was a chap who'd managed to simultaneously choke on lunch, vomit everywhere, aspirate and start fitting. Cue real ITU action involving securing the airway by RSI and intubation, which was made much more difficult by the resurgence of lunch from the lungs. Much suctioning later and he was ready for an arterial line placement and transfer to CT for a brain scan. The chap was ventilated on ITU overnight and extubated this afternoon and not looking too bad. His lunch continues to resurface periodically.
Conclusion - hospital lunches are dangerous.
Saturday, 6 August 2011
Dr Doctor please speak to the family.
In elderly care a lot of bad news tends to get broken. A lot of patients sadly come to the ends of their lives on these wards, mostly because they've just been living for a very long time and have diminished reserves and multiple co-morbidities.
One lady of 95 was admitted with a stroke a couple of weeks ago and managed to acquire an infection of some sort. She was really very unwell and probably coming to the end of her life and it fell to me to talk to the family about possibly going down the palliative care route if she deteriorated further. I had mixed feelings about being the one to do this. On one hand, I probably knew her the best out of my junior doctor colleagues, but then I am the most junior of my junior doctor colleagues. It's a powerful position to be in, with the family looking to you for answers to their questions, and to have the authority to explain that we wouldn't continue active treatment if their mum takes a turn for the worse. I felt slightly out of my depth, as it wouldn't be my decision to discontinue active treatment, and as I'd only been a real doctor for two days had never had the opportunity to lead such a conversation before. If I said the wrong thing in the wrong way the whole encounter could go horribly wrong and the family's faith in me and in our team could be diminished.
So I fell back on my commuication skills teaching from medical school. Step 1: find out what they know already. This turned out to be a good strategy because it meant the relatives actually did all the talking for a good 5 minutes. Cue an outpouring of the story so far and their feelings, which allowed me to pick up on the fact they already knew she was DNAR and they already knew she'd had a very big stroke, and they already knew she was very unwell. This gave me a good link to start talking about "if things get worse, keeping her comfortable", which they took on board very well. I was also able to explain what were doing for her in terms of treating the infection, which gave them some reassurance that we hadn't given up on her.
One lady of 95 was admitted with a stroke a couple of weeks ago and managed to acquire an infection of some sort. She was really very unwell and probably coming to the end of her life and it fell to me to talk to the family about possibly going down the palliative care route if she deteriorated further. I had mixed feelings about being the one to do this. On one hand, I probably knew her the best out of my junior doctor colleagues, but then I am the most junior of my junior doctor colleagues. It's a powerful position to be in, with the family looking to you for answers to their questions, and to have the authority to explain that we wouldn't continue active treatment if their mum takes a turn for the worse. I felt slightly out of my depth, as it wouldn't be my decision to discontinue active treatment, and as I'd only been a real doctor for two days had never had the opportunity to lead such a conversation before. If I said the wrong thing in the wrong way the whole encounter could go horribly wrong and the family's faith in me and in our team could be diminished.
So I fell back on my commuication skills teaching from medical school. Step 1: find out what they know already. This turned out to be a good strategy because it meant the relatives actually did all the talking for a good 5 minutes. Cue an outpouring of the story so far and their feelings, which allowed me to pick up on the fact they already knew she was DNAR and they already knew she'd had a very big stroke, and they already knew she was very unwell. This gave me a good link to start talking about "if things get worse, keeping her comfortable", which they took on board very well. I was also able to explain what were doing for her in terms of treating the infection, which gave them some reassurance that we hadn't given up on her.
Dr Doctor what about fluids?
Day two and I'm getting the hang of prescribing fluids. Essentially working on the principle that low sodium => normal saline, high sodium => dextrose (but make sure they have some saline at some point, and some potassium at some point) and low potassium => haartman's. If patient on certain drug regime that needs certain fluids, refer to nurses. Maintenance fluids in fit young patient 8 hourly, fluids in small, frail patient with CCF 12-18 hourly. If 1L bag finishes in the middle of the night write up another bag so night team arent bothered by unnecessary bleeping. Seniors, feel free to comment with additional advice.
Had episode of SVT upon spotting the "shit's above the seagull sign" (as in, pulse rate higher than systolic BP) on a little old lady's chart. Informed registrar who suggested I assess her for fluid balance. Wasnt quite sure what this meant but went to examine her. She was GCS 15 and looked well. Heart rate (at palpable radial pulse) was not as high as obs suggested. BP was not as low as obs suggested. BP did not decrease on standing (in fact in increased which is good going for an 80 year old). Tongue looked dry and skin turgor was decreased, cap refill was 3 secs. So she wasn't shocked but needed fluids. My heart rate returned to normal.
Had episode of SVT upon spotting the "shit's above the seagull sign" (as in, pulse rate higher than systolic BP) on a little old lady's chart. Informed registrar who suggested I assess her for fluid balance. Wasnt quite sure what this meant but went to examine her. She was GCS 15 and looked well. Heart rate (at palpable radial pulse) was not as high as obs suggested. BP was not as low as obs suggested. BP did not decrease on standing (in fact in increased which is good going for an 80 year old). Tongue looked dry and skin turgor was decreased, cap refill was 3 secs. So she wasn't shocked but needed fluids. My heart rate returned to normal.
DrDoctor dont you know anything??
And here it is, Wednesday 3rd August, affectionately known as the Day of Death amongst seasoned nurses and senior clinicians, when all the brand new F1 doctors are let loose on the wards. Having spent five years pretending to be a doctor and one month in limbo between finals results day and officially starting work amused at being called Dr Doctor by friends and family, to find myself with vast quantities of responsibility in the form of prescription writing (as in, authorising the administration of a substance that will actually change that patient's physiology), assessing patients (as in, in order to decide what on earth to do with them) and writing in the notes (as in, without the understanding that signing off as a medical student would mean everything I had written would be entirely disregarded by anyone wanting to know something relevant about the patient). Naturally I had spent my entire month off celebrating, being on holiday, and forgetting everything I had learnt for finals. I did however find the above diagram helpful.
What I hadn't realised, was that not only were all the F1 doctors starting, all the SHOs were changing jobs as well. So everyone I had got to know during Shadowing Week (usually unpaid opportunity to practise how to look dazed and confused on ward rounds, run around in a disorganised fashion trying to find forms you have never seen nor heard of, and remind oneself what patients look (and smell) like) had disappeared and somehow I became the junior doctor that new the most about how our particular ward/hospital worked.
I found myself accosted by a nurse informing me that "the patient's heart rate has gone up". "How high?" I asked, frantically trying to remember something about this particular patient. "130". The nurse then looked at me, clearly expecting me to know what action to take. "Er.. maybe needs an ECG?" Having made the nurse look satisfied with a vaguely sensible answer she disappeared, and came back brandishing said ECG at me. Thankfully my pattern recognition kicked in and I spotted he was in fast AF. And then I found myself checking the notes for a previous ECG (it was new AF), assessing him for conscious level, SOB, chest pain and signs of shock and concluding (having checked with the friendly registrar) he was probably stable enough to go for the CT that the porters were hovering about waiting to take him down for. Cue long 40mins with intermittent imaginings of him arresting in the scanner. Wrote up digoxin and vowed to take blood (to check for electrolyte disturbances and markers of infection, did he have a CXR?). Patient returns alive and back in sinus rhythm. Crossed off digoxin and breathed sigh of relief. Maybe this whole responsibility thing wont be so bad after all..
What I hadn't realised, was that not only were all the F1 doctors starting, all the SHOs were changing jobs as well. So everyone I had got to know during Shadowing Week (usually unpaid opportunity to practise how to look dazed and confused on ward rounds, run around in a disorganised fashion trying to find forms you have never seen nor heard of, and remind oneself what patients look (and smell) like) had disappeared and somehow I became the junior doctor that new the most about how our particular ward/hospital worked.
I found myself accosted by a nurse informing me that "the patient's heart rate has gone up". "How high?" I asked, frantically trying to remember something about this particular patient. "130". The nurse then looked at me, clearly expecting me to know what action to take. "Er.. maybe needs an ECG?" Having made the nurse look satisfied with a vaguely sensible answer she disappeared, and came back brandishing said ECG at me. Thankfully my pattern recognition kicked in and I spotted he was in fast AF. And then I found myself checking the notes for a previous ECG (it was new AF), assessing him for conscious level, SOB, chest pain and signs of shock and concluding (having checked with the friendly registrar) he was probably stable enough to go for the CT that the porters were hovering about waiting to take him down for. Cue long 40mins with intermittent imaginings of him arresting in the scanner. Wrote up digoxin and vowed to take blood (to check for electrolyte disturbances and markers of infection, did he have a CXR?). Patient returns alive and back in sinus rhythm. Crossed off digoxin and breathed sigh of relief. Maybe this whole responsibility thing wont be so bad after all..
Subscribe to:
Comments (Atom)